Don’t let your patients go untreated for mood distress.
Your coding of Section D — Mood — could make the difference between residents getting the care and treatment they need and continued suffering. After all, what you really do while coding this section is to make your physicians aware of the presence or absence of certain mood indicators. With quality of care being a major factor in the time ahead, you simply can’t afford to ignore this section and avoid surveyor scrutiny.
“Mood distress is a serious condition that is underdiagnosed and undertreated in the nursing home,” Brenda Sowash, BSN, RN, RAC-CT of Rolf Consulting LLC said in a recent presentation for Leading Age Michigan. Mood problems are associated with significant morbidity, but the “signs and symptoms of mood distress are treatable — treatments are very effective.”
Remember: By coding Section D, you are not making a diagnosis of mental illness. “Coding the presence of indicators does not automatically mean a diagnosis of depression or other mood disorder,” Sowash noted.
“Assessors do not make or assign a diagnosis in Section D,” agreed Beckie Dow, RN, RAC-MT, Director of MDS/Nursing Education & Training for Harmony Healthcare International Inc., in a recent training session. Your job is to “simply record the presence or absence of specific clinical mood indicators.”
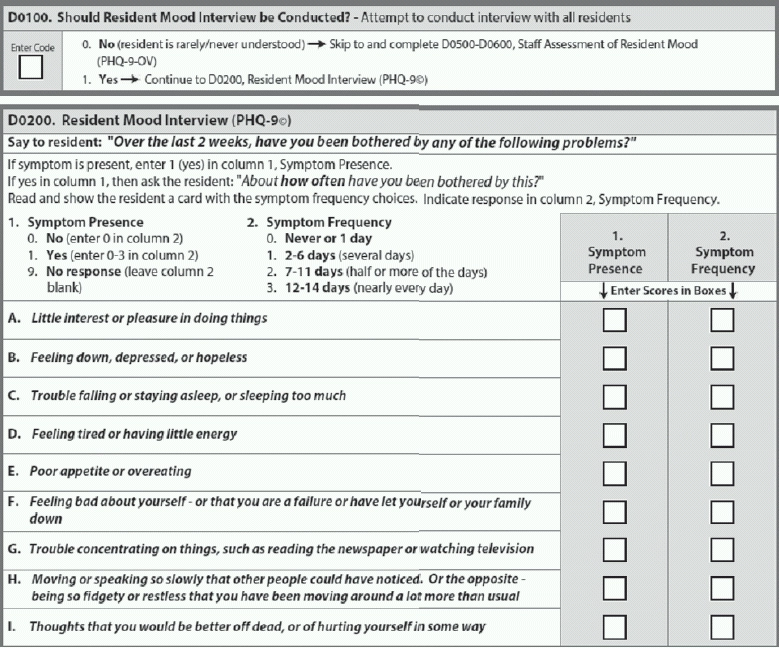
Even if you have your doubts about a resident’s ability to communicate effectively, you should attempt the mood interview with all residents, except for those who are “rarely or never understood.” Most residents are able to attempt the mood interview, so “attempt to conduct the interview with all residents if at all possible,” Sowash said.
If the resident is rarely or never understood, code D0100 — Should Resident Mood Interview Be Conducted? as 0 — No and skip to the Staff Assessment of Resident Mood. For all others, code this item as 1 — Yes and continue on to code D0200 — Resident Mood Interview (PHQ-9©).
Don’t Be Afraid to Ask about Self-Harm
When coding D0200, you must code the higher frequency if the resident has difficulty choosing between two selections, Sowash instructed. Also, do not define for the resident, and you should code 9 — No response for any nonsensical responses.
You must record the resident’s responses as he states them, regardless of whether the resident or you attribute the symptom to something other than mood, Dow urged. The responsible clinician has the task of evaluating the clinical relevance of the resident’s reported symptoms further.
The hard question on the PHQ-9© is D0200I — Thoughts that you would be better off dead, or of hurting yourself in some way, Sowash noted. But you have to ask the resident about suicidal thoughts as part of the mood interview.
Strategy: “Ask the question openly and without hesitation,” Sowash advised. Experience with this question indicates that residents appreciate the opportunity to express these types of feelings and thoughts. And asking this question does not give residents any ideas toward self-harm.
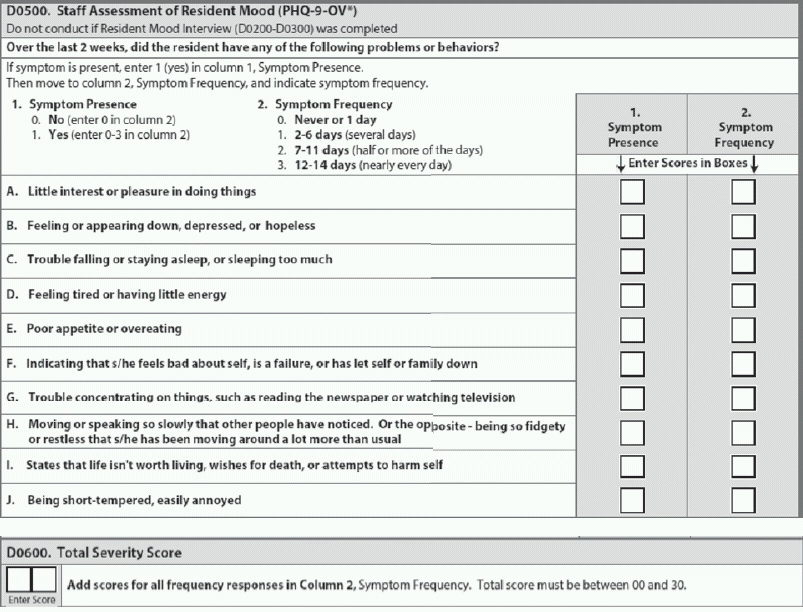
How to Tackle the Staff Assessment
When completing Item D0500 — Staff Assessment of Resident Mood (PHQ-9-OV©), remember that the look-back period is 14 days. If the resident has been in the facility for less than 14 days, talk to his family members or significant other and review his transfer records, Sowash instructed. Also, ask staff members to “select how often a symptom occurred during the look-back period.”
Note: You’ll notice that the same sub-items appear in D0500 as in the PHQ-9©, with the addition of the item about the resident being short-tempered and easily annoyed (D0500J — Being short-tempered, easily annoyed), Sowash said. PHQ-9-OV© is the “observational” version of the mood assessment.
Keep in mind that although PHQ-9© is a single point-in-time interview, the staff assessment version PHQ-9-OV© should include information from all shifts and disciplines, Dow advised. You should not rely on a single staff member’s perspective to complete Item D0500.
What the Severity Score Means for RUG Classification
You should total only the frequency items in Column 2 for the value you code in D0300 — Total Severity Score. The score will be between 00 and 27, and your MDS computer software will calculate the Severity Score for you, Sowash noted. For the PHQ-9-OV© score in Item D0600, the value will be between 00 and 30.
These scores are important in giving you and other key staff a perspective of the resident’s mood status over time, in terms of whether the resident’s mood is improving or getting worse, Sowash said. The Severity Score is critical for care planning as well as reimbursement — if the score is greater than or equal to 10 but not 99, the result will impact 26 RUG groups.
The PHQ-9 scoring for severity determination is as follows:
Go Beyond Section D Coding
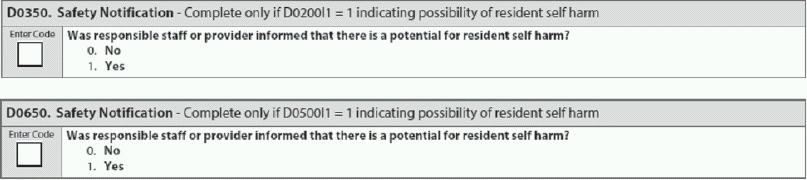
Finally, Item D0350 — Safety Notification (or staff assessment Item D0650) acts as a reminder to take appropriate action if a resident expresses mood distress.
“Untreated depression can cause significant distress and increased mortality beyond the effects of other risk factors,” Sowash warned. “Although rates of suicide have historically been lower in nursing homes, indirect self-harm and life-threatening behaviors are common.”