Reader Questions
Question: What’s the proper way to document respite care in the MDS 3.0?
Answer: “Respite refers to short-term, temporary care provided to a resident to allow family members to take a break from the daily routine of caregiving,” explains the Oklahoma State Department of Health (OSDH) Quality Improvement & Evaluation Service. For all respite residents, you must complete an Entry tracking record and a Discharge assessment.
If the respite stay is 14 days or longer, you must complete an Omnibus Reconciliation Act of 1987 (OBRA) Admission assessment, OSDH instructs. Also, you must complete the care plan seven days after you complete the admission assessment (RAI Manual, page 2-14). And don’t forget to initiate an interim care plan to guide staff in resident care if the admission OBRA assessment is not yet completed.
Question: When a resident has dentures or a partial, do I need to check L0200B?
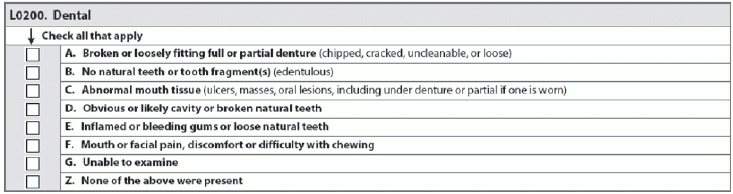
Answer: You should check L0200B — No natural tooth or tooth fragment(s) (edentulous) if the resident is edentulous or lacks all natural or parts of teeth, said Carol Siem, MSN, RN, GNP-BC, RAC-CT, Educator and Team Leader for the Quality Improvement Program for Missouri’s Long-Term Care Facilities (QIPMO).
L0200B is not asking if the resident has dentures, which is addressed in the previous question, L0200A — Broken or loosely fitting full or partial denture (chipped, cracked, uncleanable, or loose), Siem noted. Instead, L0200B is asking if the resident has any teeth at all.