Long-Term Care Survey Alert
Here's How to Ensure a Compliant Return To Community
Your resident’s individual rights come first.
Coding a resident’s desire to return to the community in Section Q of the MDS doesn’t have to be a hassle, even if your facility staff doesn’t think that’s a good idea. Your concern for the facility’s liability, particularly for follow-up care, is legitimate. Here’s how you can ensure a smooth transition.
Consider this case study, used in a past MDS National Conference held by Washington, DC-based Leading Age, to get a grasp on what to do.
Scenario: Mrs. Smith is an elderly woman who has been blind since birth. She lived with her parents until she was married, and then lived with her husband until he passed away. Mrs. Smith moved into a nursing home about five years ago, because she has always been terrified to live on her own. She now uses a wheelchair 100-percent of the time.
Despite being previously scared to live on her own, Mrs. Smith responded “Yes” to item Q0500B — Return to Community on her annual MDS assessment. She is an active and very social person and said that she desperately wants to leave the facility to live independently. Mrs. Smith has no appointed legal representative.
Snag: But Mrs. Smith’s physician and the social worker at her nursing facility are very reluctant for her to leave the facility. They are concerned about her safety while living alone, as well as for her ability to take care of her activities of daily living (ADLs) because the staff had done all of that for her in the facility.
Consider These 7 Questions to Proceed
1. Who has the right to make this decision? Mrs. Smith has the right to make this decision, because in this scenario there is no evidence of a legally authorized (court appointed) representative. The physician or social worker has no legal standing to make this decision. They can offer advice and share their concerns, but they cannot interfere with Mrs. Smith’s decision.
2. Does Mrs. Smith have the right to take the risk of moving out of the nursing facility? Yes, Mrs. Smith has the right to make her own medical decisions, including the right to accept or refuse medical services and settings.
Understand Related Liability Concerns
3. What is the nursing facility’s liability after Mrs. Smith is discharged? Although Mrs. Smith is a resident in the facility, the nursing facility is responsible for a thorough assessment of the individual resident’s needs, supporting the resident in achieving her highest level of functioning, discharge planning, and implementing the discharge plan. The facility should work closely with the community agency — local contact agency (LCA) or service provider — that is providing transition planning and arranging community supports and services such as housing, transportation, personal care assistance, and other formal and informal supports.
When you develop a discharge plan that prepares the resident for discharge into the community, there should be a smooth transition. You must consider meeting the resident’s needs in the environment, availability of resources to provide care, treatment, etc., and educating the agency providing oversight of the resident’s specific needs and how they are to be met.
Resident protections concerning transfer and discharge are found at §483.12: A “post-discharge plan of care” means the discharge planning process, which includes assessing continuing care needs and developing a plan designed to ensure the individual’s needs will be met after discharge from the facility into the community.
Bottom line: After appropriate implementation of the nursing facility discharge plan, once the individual is smoothly discharged, the nursing facility is no longer responsible for the individual’s care. If the resident is Medicaid-eligible, the community service providers and the State Medicaid Agency are responsible for assuring health and safety once the individual has transitioned back to the community.
Remember Your Residents’ Rights
4. What is the nursing facility’s liability if Mrs. Smith responds “Yes,” but the assessor marks “No?” The nursing facility is required to make a referral to the LCA and work with the LCA in a person-centered approach to explore the resident’s options for supports and services in the community and the possibility that the resident may return to the community. Federal law and regulation 42 CFR 483.20(i)(3) requires that your facility continues to implement accurate discharge planning and follow-up.
5. If a competent individual resident determines that she wants to talk to someone about returning to the community, does the nursing facility have the right to block the LCA from seeing the resident? No. The U.S. Supreme Court decision in Olmstead v. L.C. and the Americans with Disabilities Act require that residents have access to information and choices. LCAs are designated by State Medicaid Agencies officials as part of a structured discharge-planning process.
Code Section Q Items This Way
6. How would you code Q0500B? What steps are then required? In this scenario, you would code Q0500B as “Yes” (1). The “Yes” response will trigger follow-up care planning and discharge planning, and contacting the LCA according to your state’s protocols, usually within 10 business days.
7. How would you code Q0600 — Referral? What steps are then required? You would code Q0600 as “Yes — referral made” (2). You would then begin the appropriate care planning and discharge planning. Once the LCA talks with the resident and facility, if the LCA determines that there are supports and services that would enable the resident to return to the community, work with the LCA and/or designated agency on other follow-up measures.
Long-Term Care Survey Alert
- Patient Privacy:
Hidden Cameras: Protect Residents' Privacy -- And Your Reputation -- In The YouTube Era
Electronic monitoring could spell trouble at survey time. Headlines these days are laden with words [...] - MDS Section Q:
Here's How to Ensure a Compliant Return To Community
Your resident’s individual rights come first. Coding a resident’s desire to return to the community [...] - Cover The Bases With This Electronic Monitoring Checklist
Does the facility want to provide for electronic monitoring? If so, what devices will the [...] - Are Cameras a Good Idea in Your Facility?
Weigh these video surveillance pros and cons. Consider these pros and cons as you grapple [...] - Care Area Assessment:
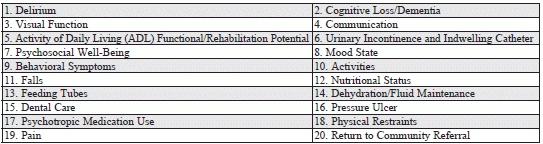
Delve Deeper Into Those CATs
Don’t expect your MDS software to do all the work for you. Being able to [...] - Change Management:
Prepare Employees For Change With 6 Strategies
Change is inevitable in any organization. So is resistance to change. Getting your nursing facility [...] - Industry News
Nix Your Facility-Wide ‘No CPR’ Policy You’ll end up in hot water with the Centers [...]

