Prolonged Services Codes Can Generate Extra Pay With E/M Services

Document accurate E/M time to get maximum deserved reimbursement.
Whenever your clinician performs an E/M service, don’t miss out on opportunities that arise in the form of prolonged services to get additional reimbursement for the extra time and efforts that your internist spends in the patient’s evaluation and management.
Review these three tips to gain a better understanding of how to accurately determine the E/M and prolonged service times, so you never miss an opportunity to legitimately report prolonged services.
Breakdown the Time Spent After the 30-Minute Threshold
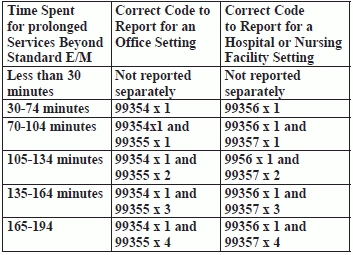
When your provider sees a patient for an extended period of time and an E/M visit code alone doesn’t accurately represent the service he provided, you may be able to report an additional prolonged service code. You will choose from the following codes based on the place of service and the time spent:
To determine the correct prolonged services code you should report, look at the time your provider spent on prolonged services with face-to-face patient contact and compare that to the typical time of the base E/M code you are otherwise reporting (i.e., the reference time). Without the reference time, there’s no way to define a service as prolonged. Refer to the quick reference table to use the time spent during the service to determine the correct add-on code for the prolonged service.
Key: “Any prolonged E/M service code is not reportable if the prolonged service is less than 30 minutes beyond the typical time of the base E/M code,” says an expert. In other words, your provider has to cross the 30-minute threshold time before the prolonged services codes kick in. So once the time with the patient goes over the threshold time, you can use a prolonged service code. If, however, the physician spends less than 30 extra minutes with a patient, you will not use +99354-+99355 or +99356-+99357.
Example: A new patient comes into your office and your internal medicine specialist spends 120 minutes in this patient’s evaluation. Because most of that time was spent on counseling and coordination of care and your provider documented appropriately for time-based billing, you code 99205 (Office or other outpatient visit for the evaluation and management of a new patient …) for the E/M service; code 99205 typically involves 60 minutes of face-to-face time with the patient. Since the physician spent a total of 120 minutes with the patient, the prolonged service portion was 60 minutes (i.e., 120 minutes total minus 60 minutes associated with 99205). Since the prolonged portion exceeds the threshold of 30 minutes, you can report a prolonged services code in addition to 99205. In this instance, you can also report +99354 for this encounter.
Important: You can report only one unit of either +99354 or +99356 per date of service, but you can report multiple units of +99355 or +99357 per day. You cannot report +99355 without first reporting +99354, nor can you report +99357 without first reporting +99356.
Count Contact Time on Same Day
When counting the time spent on an encounter for determining whether you can report a prolonged services code, the face-to-face patient contact doesn’t have to be continuous but it does have to be on the same day. “In the office or other outpatient setting, Medicare will pay for prolonged physician services (+99354) when billed on the same day by the same physician or qualified NPP as the companion E/M codes,” Mehalich advises.
Example: Your internist sees an established patient in a morning office visit (99213, Office or other outpatient visit for the evaluation and management of an established patient, …15 minutes …) to determine the cause of chronic heel and ankle pain. This visit lasts 30 minutes. At the end of the exam, your clinician orders an x-ray. The patient leaves to get the x-ray and returns that afternoon. Your physician reviews the x-ray with the patient and discusses his diagnosis and treatment options. This visit lasts 30 minutes.
Code it: You would use 99213 and add-on code +99354, even though the time spent by your physician with the patient wasn’t continuous.
“Medicare will pay for a prolonged visit if it is billed on the same day by the same physician or qualified NPP, if the time was spent discussing treatment options with patient/family” adds Dawn J. Lafferty, MPA, CMRS, CRA, RMA, faculty at Bryant and Stratton College in Rochester, N.Y. “We need to be careful that a prolonged visit is not coded if the time was spent reviewing the chart, waiting for lab results, or the patient spent a significant amount of that time with office staff.”
Tie Your Claim with a Bow
To support your use of prolonged services codes, you need to explain why the physician needed to provide a prolonged service. Just saying the physician spent 47 minutes with the patient isn’t sufficient enough to keep the claim from being denied when your payer asks for documentation to review. You need proof of medical necessity.
If your physician hasn’t provided medical necessity for the prolonged service in his notes, you can either talk to him to get the detailed information that you need in order to complete your coding or consider skipping the prolonged service code. If you can’t report +99354-+99357 because of limited documentation, you may want to educate your physician on the monetary benefit to him if he better documents face-to-face time and medical necessity for extended encounters.
Caution: You also don’t want to overuse prolonged service codes. According to CMS estimated usage rates, on average, code +99354 is reported only about once every 1,000 claims, and code +99356 is reported only about once every 100,000 claims. If your usage is significantly greater than that average, it may prompt a review at some point.