Use This Guide to Perfect Lesion Excision Coding
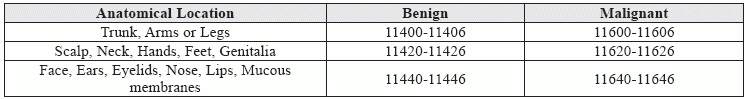
Here’s when you might be able to report excision and wound closure. If your internist excises a patient’s skin lesion, you will need to know whether on not to wait for the pathology report to accurately report the procedure that your clinician performed. Further, you need to focus on other factors that you need to consider to help you zero in on the right code. Use this guide to help hone your lesion excision coding. Find Anatomical Location First When your clinician performs an excision of a lesion, you can zero in on the code range by checking on the anatomical location of the excision. Keep this charthandy as you look for the appropriate CPT® code range. Check Type of Lesion First you have gone through the patient chart notes to find the anatomical location from which your clinician excised the lesion. Next, you will need to look for the diagnosis that your clinician has made from the case history as well as from the pathology report. Don’t rely entirely on your clinician’s observations in deciding the lesion type because you might end up using a benign code for a malignant lesion or vice versa. If the lesion on visual exam appears consistent with a benign growth but is ultimately malignant and if you reported a benign lesion excision, you might end up losing on deserved pay. You will have received a lesser reimbursement as malignant lesion excision codes pay higher than excision of benign lesions of the same size in the same anatomical location. On the other hand, if on visual examination your clinician determines that the lesion is malignant while the path report counters the claim and says that the lesion is actually benign, you will be committing an error in reporting and may end up raising unwarranted red flags. “It is always best to wait for the pathology report before billing out the excision,” says Mary I. Falbo, MBA, CPC, CEO of Millennium Healthcare Consulting, Inc. in Lansdale, PA. So, do not just rely on what your clinician has determined the lesion to be based on visual examination but report the procedure only after receiving the path report. “Most pathology reports are available within 24 hours, so this should not pose a problem,” Falbo adds. Note: If the path report concludes that the lesion is benign or shows signs of atypia, dysplastic changes, or any other uncertain behavior, you will have to report the lesion with a benign code while you report the lesion as malignant if the report says that the lesion is malignant (primary or secondary) or in-situ. Determine Excision Size After having determined the anatomical location from which the lesion was removed and the lesion type, you will need to then shift focus to the size of the excision. This will help you zero in on the right code that you will report for the procedure. “Code selection is determined by measuring the greatest clinical diameter of the apparent lesion plus that margin required for complete excision,” according to CPT® guidelines. So, in order to determine the size of the excision, you will need to check the diameter of the lesion and determine the narrowest margin that is needed to adequately excise the lesion. “That’s why the descriptor for these codes says, ‘Excision, [benign/malignant] lesion including margins,’” says Kent Moore, senior strategist for physician payment at the American Academy of Family Physicians. In other words, the size of the excision will be equal to the longest determined length of the lesion added to two times the narrowest margin. Caveat: Don’t determine the size of the excision based on what the pathology report mentions the size of the lesion to be. You need to remember that lesions shrink when the pathologist analyzes them and you might lose out on reimbursement if you determine the size of the lesion from the path report. In order to determine the size of the excision correctly, you should get your clinician to measure the lesion as well as the margins before performing the actual excision. In addition, you should remember that size of the lesion should not be determined using the length of the incision that your clinician performed or the length of the surgical wound. Know When to Report Wound Closure When your clinician performs an excision of a lesion, you also need to know whether you should separately report closure of the surgical wound after the procedure is completed. If your clinician only performed a simple closure of the surgical wound, you won’t report it with an additional code. Simple closure is inherent to the excision code that you’ll report for the procedure. On the other hand, if your clinician performs an intermediate or a complex repair, you will need to report the closure with an appropriate repair code. For intermediate repairs, report an appropriate code from the CPT® range, 12031-12057 depending on the length of repair and the anatomical location. For complex repairs, choose from the CPT® range, 13100-13153 again depending on the location and length of the repair performed. “Be aware that the groupings of anatomical location for intermediate and complex repairs are not the same as those for lesion excision,” Moore says. “For example, the trunk and scalp are in separate anatomical region categories for lesion excision but lumped together for purposes of intermediate repair.”