Internal Medicine Coding Alert
Take These Four Hints to Master Skin Procedure Coding

You don't have to dig too deep to understand biopsies, removals and excisions.
On the surface, documenting skin excisions, shave removals, or biopsies is pretty straightforward, especially when you follow these four basic pointers:
- What was the removal's purpose?
- How deep was the incision?
- Where on the patient's body was the procedure performed?
- How big was the incision?
Each one will help lead you to the code that most accurately describes the specific procedure your internist has performed upon a patient.
Zero in on Purpose
Generally speaking, when your provider removes a section of skin from a patient's body, he or she is attempting to diagnose a problem, to relieve a condition or, in some cases, both.
For biopsies, you really only have two codes to choose from: 11100 (Biopsy of skin, subcutaneous tissue and/or mucous membrane (including simple closure), unless otherwise listed; single lesion) and the add-on code 11101 (...each separate/additional lesion (List separately in addition to code for primary procedure)) if your provider is removing additional lesions for multiple biopsies.
If you do report either of these codes, you should remember that CPT® guidelines clearly state they are to be used when the purpose of the procedure is for biopsy only. The other shaving and excision codes have biopsies built in, so coding 11100/11101 along with an excision or shaving code for the same lesion is not only redundant, it's also reason for denial or audit.
Kent Moore, senior strategist for physician payment at the American Academy of Family Physicians, notes that coders can get tripped up by the terminology describing the procedure. Moore offers the example of the term "shave biopsy." "If coders are not careful," Moore cautions, "focusing on the word 'shave' may lead them to report a shave removal when, in fact, the key word is 'biopsy,' which leads to this different set of codes."
Moore also points out that, under certain circumstances, biopsy codes can be reported with shaving or excision codes.
"It is possible and acceptable," Moore notes, "to biopsy a site on one part of the body, such as the right arm, and shave or excise another lesion on a different part of the body, such as the left arm." To code this, Moore suggests using an appropriate modifier, such as modifier 59 (Distinct Procedural Service) along with appropriate diagnosis codes, which may distinguish location and or laterality for the different lesions involved.
Determine Depth for Accuracy
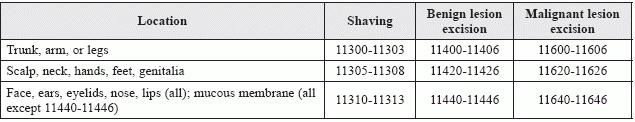
CPT® distinguishes between two different procedures for lesion removal: shaving (codes 11300-11313) and excision (codes 11400-11646). Shaving is performed on the top two layers of the skin, the epidermis and the dermis, while excisions go deeper than those layers and into the subcutaneous tissue below.
Not only does this definition help pinpoint the correct code, but it can also help identify the need for other codes. Moore notes that as shaving does not require a suture closure, no closure codes are generally reported. But, Moore adds, excisions need to be closed. A basic excision procedure "includes simple closure," Moore notes, "whereas intermediate and complex closures are separately reportable" with 12031-12057 for intermediate closures or 13100-13153 for complex closures.
Check Location for these Procedures
Both shaving and excision codes are grouped by location, as can be seen in the table at the end of this article.
However, these may not be the best codes to describe the procedure your provider may perform. Melanie Witt, RN, CPC, MA, an independent coding expert based in Guadalupita, New Mexico, reminds coders that other "site-specific biopsy or soft tissue excision codes may better describe a procedure than standard integumentary biopsy or excision codes."
Measuring Size? It Might Not Be So Simple
Each of these shaving and excision codes are subdivided by size, with dimensions built into the code descriptors for fast reference. For a shaving code, such as 11300 (Shaving of epidermal or dermal lesion, single lesion, trunk, arms or legs; lesion diameter 0.5 cm or less), a simple diameter is included in the descriptor, making it easy to find the correct code.
Excision codes, however, are a little trickier, as CPT® guidelines require the diameter to be calculated with an included margin. So, if your provider excises a benign lesion with a diameter of 2 cm from a patient's hand and reports leaving a 0.2 cm margin around the lesion, you would add 0.4 cm (0.2 cm x 2) to the lesion diameter and report 11423 (Excision, benign lesion including margins, except skin tag (unless listed elsewhere), scalp, neck, hands, feet, genitalia; excised diameter 2.1 to 3.0 cm), as the total diameter of the excision adds up to 2.4 cm.
As a note of coding caution, however, Witt points out that "the size of the lesion and the area of the margins removed may not be documented in the procedure note." So, Witt offers the reminder that that coders need to consult with their providers "in order to get the correct size for coding purposes."
Related Articles
Internal Medicine Coding Alert
- E/M Coding:
Review These Questions, Receive ROS Answers
Use this FAQ to enhance your E/M understanding. Reporting your provider's review of a patient's [...] - Procedure Coding:
Take These Four Hints to Master Skin Procedure Coding
You don't have to dig too deep to understand biopsies, removals and excisions. On the [...] - You Be the Coder:
Report this Code for Therapeutic Stimulant Use? Think Again
Question: I have two questions about documenting periodic therapeutic drug screens, which our provider performs [...] - Clip & Save:
Locate, Use Common GI Codes Easily With This Tool
And refine your coding accuracy with some expert advice. Patients reporting with gastrointestinal (GI) conditions [...] - Reader Question:
Reduce Stress, Use This Supervision Code in This Cardio Test Scenario
Question: Our physician has been sending patients to a local hospital for stress echo testing. [...]




