Internal Medicine Coding Alert
MAC To Readjust Denials for Routine Foot Care and Nail Debridement

If you have been recently facing Medicare denials when your internist is performing routine foot care or debridement of nails, don’t fret. You may not be alone. Likewise, you may also have company if you have been recently facing Medicare denials for preoperative tests that your physician ordered. Recent information from National Government Services (NGS), a Medicare administrative contractor (MAC), discusses these problems and what you need to do if you encounter them.
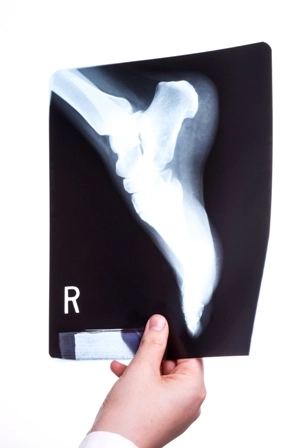
Scenarios: Your provider performed debridement of 5 nails for a Medicare patient. You reported 11720 (Debridement of nail[s] by any method[s]; 1 to 5). You face a denial to your claim. In another situation, you report 11719 (Trimming of nondystrophic nails, any number) for routine foot care that your physician performed for another Medicare patient. You got a denial for this claim, too.
In yet another situation, you face a denial for some preoperative tests (like a chest x-ray or an EKG) that your physician ordered. These tests were not routine preoperative tests but tests that your internist ordered due to medical necessity.
So, what are you doing wrong? According to NGS, you may not be doing anything wrong; the fault may lie with your MAC.
The problem: NGS has identified the following production issues that are causing erroneous denials of these types of claims.
Routine Foot Care and Debridement of Nails
Noncovered Services
What you need to do: NGS will be adjusting the denied claims for routine foot care and debridement of nails to pay correctly. No provider action is required. Also, claims for preoperative tests that have been denied incorrectly will be reprocessed by NGS. No provider action is required. If you submit your claims to a MAC other than NGS and are having the same problems, please check with your MAC to see if any action is needed on your part to correct the situation or if your MAC will make the necessary adjustments on its own.
Related Articles
Internal Medicine Coding Alert
- Influenza Vaccine Update:
Strengthen Your Influenza Coding Knowledge With 90630
Heads up: The code is now FDA-approved, so expect payments Although the influenza vaccine code [...] - NGS Update:
MAC To Readjust Denials for Routine Foot Care and Nail Debridement
Watch out for scenarios where Medicare is denying payments for preoperative tests, too. If you [...] - ICD-10:
ICD-10 Transition Sailing Smooth For Most Practices
Some potential issues, however, may remain to be analyzed. If you asked medical practices a [...] - Clip and Save:
Influenza Coding Made Easy with These Handy Tips
As flu season drags on, you will need to be quick on your toes to [...] - Consultations:
Remove Cloud Of Doubts In Consultation Coding
Confirm with your payer before billing if it follows Medicare rules. Medicare doesn’t recognize consultation [...] - You Be the Coder:
Learn if You Need an Anesthesia Modifier With Procedural Code
Question: We had a young patient who came into our office for an ingrown toenail (11750). [...] - Reader Question:
"No Charge" Visits Count Toward Established Patient Status
Question: Our internal medicine specialist saw a patient during a quick assessment last year at no [...]