Hint: Follow similar list of inclusions and exclusions for both ICD-9 & ICD-10.
When your clinician diagnoses acute maxillary sinusitis, you have to note that you have a specific ICD-10 code to identify a recurrent form of the condition, a choice that you did not have when using ICD-9 system of codes.
ICD-9: When reporting a diagnosis of acute maxillary sinusitis, you have to report it with 461.0 (Acute sinusitis; Maxillary). You have to use the same ICD-9 code if your clinician’s diagnosis is acute antritis. You’ll use 461.0 if your clinician mentions an acute occurrence of any of the following conditions involving the accessory nasal sinuses:
Reminder: You cannot use 461.0 if your physician diagnoses the patient to be suffering from chronic or unspecified sinusitis. In this case, you will use a different code range that is available. You report it with the codes 473.0-473.9.
ICD-10: When you begin using ICD-10 codes, a diagnosis of acute maxillary sinusitis that you report with 461.0 in ICD-9 crosswalks to J01.0 (Acute maxillary sinusitis). As in ICD-9, you report the same diagnosis code if your clinician records the diagnosis as acute antritis.
The ICD-10 code J01.0 expands into two more codes allowing you more specificity in reporting the diagnosis if the acute maxillary sinusitis that the patient is experiencing is a recurrent condition. The two codes that J01.0 expands into include:
In other words: If your physician diagnoses the condition that the patient is suffering from as acute recurrent maxillary sinusitis, you can report the diagnosis very specifically in the ICD-10 coding system with J01.01. This option of reporting a recurrent form of the maxillary sinusitis is not available in ICD-9. Here you will only report it with 461.0 irrespective of whether the condition is an initial episode or has been a recurring phenomenon.
Check These Basics Briefly
Documentation spotlight: Your clinician will arrive at a diagnosis of acute maxillary sinusitis based on a thorough history and medical examination, including a notation of associated signs and symptoms and findings of any diagnostic tests ordered or performed.
When recording the history of the patient, your clinician will try to note details of any allergies, other medications that the patient is currently on, past medical history, and occupational history. These details will help your physician rule out other conditions that may mimic signs and symptoms that are prevalent in a patient suffering from acute maxillary sinusitis.
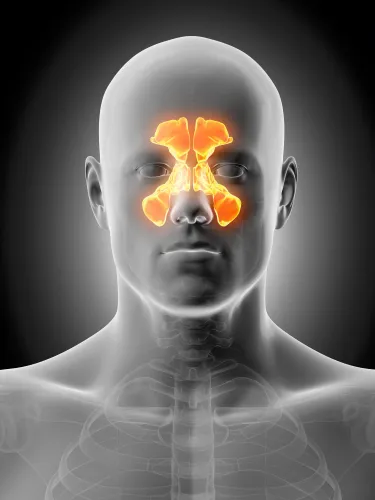
The history and interpretations of the signs and symptoms the patient is currently suffering from usually helps your clinician arrive at a diagnosis of acute maxillary sinusitis. Some of the signs and symptoms that the patient with acute maxillary sinusitis might be present with include pain over the upper maxillary teeth, redness of the area over the sinus, facial pain, persistent cough, referred pain to other areas of the face and head, blocked nose, high fever, and postnasal discharge.
Upon examination of the patient, your internist might note presence of a purulent secretion in the nose and the pharyngeal area, tenderness over the sinus area, and erythema of the nasal mucosa.
Tests: In most cases, your clinician will use the history, signs and symptoms to arrive at the diagnosis of maxillary sinusitis. But, in some cases your clinician might want to perform lab tests and diagnostic tests to rule out other conditions and to ascertain the cause for the sinusitis. Your clinician will withdraw a blood sample to be sent to the lab for analysis to see if there is any other cause for the condition the patient is experiencing and to check if the patient has decreased immune status.
Your clinician will also rely on imaging studies such as the Waters view x-ray examination of the occipito-frontal area to check the maxillary sinus for signs of opacification or thickening of the mucosa. These findings, if present along with other presenting signs and symptoms, will help your physician confirm the diagnosis of acute maxillary sinusitis. In certain cases, your clinician will also ask for a CT scan to confirm a diagnosis.
Your clinician might also rely on endoscopic studies such as sinus endoscopy or the endoscopy of the respiratory tract to confirm the diagnosis and also to collect nasal secretions that can be sent to the lab for analysis to help clinch the diagnosis of acute maxillary sinusitis.
Example: Your internist assesses a 17-year-old female patient who has been suffering from signs of acute upper respiratory tract infection. The patient had signs of URI for about a week, after which it seemed to resolve, but then again it seemed to get worse. Your physician had seen the patient a week earlier for her URI and had prescribed her medications. The patient complains of having a blocked nose, pain over her upper teeth, intermittent fever, cough, facial pain, and discharge from her nose.
Upon examination of the patient, your clinician notes purulent nasal discharge and tenderness over the maxillary sinus area. Using directed light, your clinician notes purulent secretions when examining the middle meatus with a nasal speculum. He also notes erythema of the nasal mucosa.
Based on the signs and symptoms and history of persistent and worsening of symptoms, your clinician diagnoses acute maxillary sinusitis.
What to report: You report the office visit with 99213 (Office or other outpatient visit for the evaluation and management of an established patient…). You report the diagnosis with J01.00 if you are using ICD-10 codes or report 461.0 if you are using the ICD-9 coding system.
