Type of Skin Lesions To Decide Your Code Choice For Destruction

Hint: Not all CPT® codes for destruction are add-on codes.
When your internist performs destruction of a skin lesion by methods such as laser, cryosurgery, electrosurgery, or curettement, you’ll have to delve deeper into patient documentation to check what type of lesion was removed. You also need to see if your internist provided any other services (such as an E/M) concurrently.
Stick to These Three Choices For Premalignant Lesions
If your physician is removing premalignant lesion(s) (see chart) using methods like laser surgery, cryosurgery, and other such means, you will have to select the appropriate code(s) from these three choices:
Coding tip: When reporting destruction of premalignant lesions and when your physician destroys up to 14 lesions, you’ll have to report the CPT® code 17000 for the first lesion. Then you’ll report the add-on code +17003 for the destruction of every other lesion, up to 13 times. “So, for example, if your physician destroys three premalignant lesions, you report 17000 once for the first lesion and +17003 two times (or with two units of service) for the other two lesions,” explains a coding specialist.
On the other hand, if your clinician destroys 15 or more lesions, you’ll have to report only 17004 and only once. Don’t make the mistake of reporting 17000 for the first lesion and then reporting 17004 for additional lesions. Code 17004 is not an add-on code.
Choose From Other Codes For Benign Lesions
When the lesions that your internal medicine specialist removes are benign lesions (see chart), you’ll have to use different codes instead of selecting from the code range, 17000-17004. In this case, you have two code choices to look at, again depending on the number of lesions removed by destruction. So, you can choose from the following two codes for benign lesion destruction:
Reminder: You’ll have to report only one code depending on the number of lesions your internist removes by destruction. If the number of lesions removed is equal to or less than 14, you’ll have to report it with 17110. If the number exceeds 14, you’ll have to just report 17111. Don’t report 17110 and 17111 together when your internal medicine provider removes more than 14 lesions.
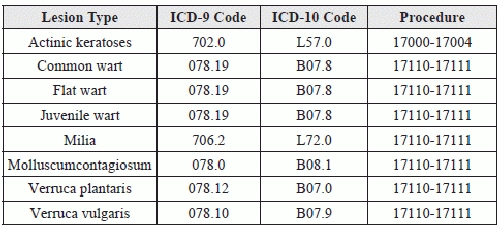
Coding tool: Use this easy reference chart to determine what destruction procedure code you should use for different types of lesions that your internist might remove.
Exercise Caution When Reporting Destruction of Different Lesion Types
Correct Coding Initiative (CCI) bundles destruction codes for premalignant and benign lesions. So, if your clinician is removing both premalignant and benign lesions, then you will hit a roadblock trying to report both these procedures together. However, the modifier indicator for these code bundles is ‘1,’ which means you can use a suitable modifier to unbundle the codes and report them separately.
As codes 17000-17004 are the ones in column 2 of the CCI edits, you will have to append a modifier to these codes when reporting them with destruction of benign lesions (17110-17111). You will append a modifier such as 59 (Distinct procedural service) to the premalignant lesion destruction code in this scenario.
Know When to Report an E/M service Separately
CCI also will not allow you to report an E/M service code in addition to destruction codes for premalignant and benign lesions, unless you append an appropriate modifier to the E/M code. So, if prior to the lesion destruction, your physician’s assessment of the patient does not exceed that otherwise included with the destruction, you will only report the destruction code.
Since the modifier indicator to the CCI bundling between destruction codes and E/M codes is ‘1,’ you will be allowed to report both these services if you use an appropriate modifier. But, you can do this only if the E/M service is significant and separately identifiable from the destruction. If the E/M service is significant and separately identifiable, you can report both the destruction and the E/M code. You will need to append the modifier 25 (Significant, separately identifiable evaluation and management service by the same physician or other qualified health care professional on the same day of the procedure or other service) to the E/M service code.
Example: An established 55-year-old female patient presents for a scheduled E/M visit to check on high blood-sugar levels for her diabetes. The patient also complains of some skin eruptions on her knees that are painful on application of pressure. During the examination, your physician finds twelve common warts in the area and advises removal immediately. The patient agrees and your internist removes the warts with laser surgery. Your physician also performs an expanded problem-focused history and exam, and medical decision-making of moderate complexity related to the diabetes, which he notes is not controlled.
What to report: The visit should be reported using 99213 (Office or other outpatient visit for the evaluation and management of an established patient…) with modifier 25 attached. The appropriate diagnosis code for the E/M visit would be 250.02 (Diabetes mellitus without mention of complication, type II or unspecified type, uncontrolled) using ICD-9 or E11.65 (Type 2 diabetes mellitus with hyperglycemia) in ICD-10.
The wart removal would be reported with 17110along with the diagnosis code 078.19 (Viral warts, other specified viral warts) in ICD-9 and B07.8 in ICD-10.