Ensure Foreign Body Removal Coding Success with These 5 Tips
Hint: Don’t use FBR codes if physician doesn’t perform an incision.
When your clinician performs a foreign body removal (FBR), you should base your reporting of the procedure depending on the depth and anatomical area at which the foreign body was located. You should also look at documentation to ascertain whether the removal was “simple” or “complicated.”
Use these five useful tips to help guide you through a step-by-step process that you will need to follow while reporting a foreign body removal.
#1 Don’t Always Reach Out to FBR Codes
When a physician performs a foreign body removal, don’t be in a hurry to report the procedure with a FBR code. First, look through documentation to see if he performed an incision or not to reach out to the foreign body. If no incision was made, then you cannot report the FBR procedure with a FBR code.
“If you look at the foreign body removal codes within CPT®, almost all of them either include the word ‘incision’ in their descriptor or they are placed in a section of the book that clearly indicates excision or some other procedure involving incision,” says a senior audit strategist.
If no incision was performed and your clinician only used an instrument such as a tweezers or a probe to either hold the foreign body or to tease it out, then it is inappropriate to report the procedure with a FBR code. In such a case, you will only reach out to the most appropriate E/M code (such as 99212, Office or other outpatient visit for the evaluation and management of an established patient ...) that will include the procedure into the other E/M services that the provider performed during the same visit.
#2 Watch Anatomical Area and Depth of FB to Choose Appropriate Codes
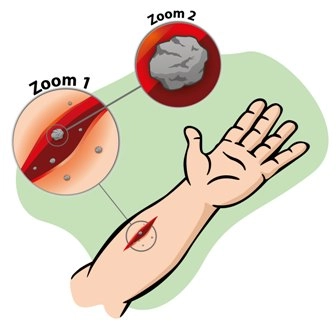
When your clinician does perform an incision to perform the FBR, you should look at the depth at which the FB was located. You will have to look through documentation to see the depth at which the FB was present as this will influence the code selection.
When the FB that the physician removed was superficial (i.e. in the skin and subcutaneous fat tissues), you will have to choose one of the following codes:
If the FB was located deeper and was found to be within the fascia, subfascial, or muscle, then you will have to report one of the musculoskeletal series of codes. For example, you might report one of the following codes:
Caveat: Before reporting one of the above mentioned codes depending on the depth of the FBR, look through documentation to see the anatomical area in which the FB was located. Checking this detail is also important as you have some site-specific FBR removal codes. For instance, if the foreign body was located in the upper arm, you have these codes to choose from:
If site specific codes are available, you should choose these codes in lieu of the generalized integumentary or musculoskeletal codes.
#3 Distinguish Between Simple and Complicated Codes
When you look at FBR codes, most of these codes carry the terms “simple” and “complicated.” These may or may not refer to the depth of the foreign body. They may be related to the complexity and time involved when an internal medicine specialist removed the FB. Refer to the physician’s documentation of the procedure when you are choosing between “simple” and “complicated.”
“In general, CPT® leaves it to the judgement of the physician to distinguish between ‘simple’ and ‘complicated,” he says.
If your clinician’s notes mentions the FBR as “simple” or “complicated,” then choose the appropriate FBR code. If there is no mention of this information, don’t be in a hurry to choose one code over the other.
If the physician was able to reach out to the FB and remove it without extensive instrumentation, then you can report the procedure with a “simple” code. On the other hand, if your clinician had to perform extensive instrumentation, exploration of the wound, or needed to use visualization and localization techniques to locate the FB and remove it, report a “complicated” FBR code. You could also report a complicated code when the removal was complicated by the presence of a complicating infection or due to the presence of any vital structures near the site.
You can look at the closure technique that your clinician used to select the appropriate code. If no closure was performed or your clinician placed simple sutures to close the site, you could report a “simple” FBR code. If your clinician performed a layered closure, then you might be justified in choosing the complicated removal code.
#4 Don’t Report FBR in Addition to Wound Exploration or Debridement
You should not report FBR if your clinician discovers and removes a foreign body during wound exploration. In such cases, the FBR is incidental to the exploration, and you would report only the exploration codes (for example, 20100-20103, Exploration of penetrating wound [separate procedure] ...).
Similarly, you should also not report FBR if your clinician finds and removes a foreign body during wound debridement. In such a case, it is best to report only the wound debridement code (for example, 11042, Debridement, subcutaneous tissue [includes epidermis and dermis, if performed]; first 20 sq cm or less), since, by common definition, “debridement” includes removal of foreign material as well as dead or damaged tissue.
#5 Support FBR Codes With Appropriate Diagnosis Codes
When reporting a FBR code, it is essential for you to report appropriate diagnosis codes to support the removal code. In order to prove medical necessity, you will need to report the appropriate diagnosis codes that identify that site and type of wound and another diagnosis code that identifies the causative factor.
So, for instance, if your clinician is removing an airgun pellet that got lodged into the patient’s right forearm due to accidental discharge, you will have to report the following two diagnosis codes to support the medical necessity of performing the FBR: