Grab the July ICD-10 Testing Opportunity by CMS
Gather tips on end-to-end testing before the official implementation date.
Cash in on the golden testing opportunity available with your Medicare contractor before the actual “go live” date later this year.
Background: During the week of July 20 - 24, 2015, a sample group of providers will have the opportunity to participate in ICD-10 end-to-end testing with Medicare Administrative Contractors (MACs) and the Common Electronic Data Interchange (CEDI) contractor.
To volunteer as a testing submitter, you need to submit the volunteer forms available at http://www.cms.gov/Research-Statistics-Data-and-Systems/Monitoring-Programs/Medicare-FFS-Compliance-Programs/Review-Contractor-Directory-Interactive-Map/
Deadline: Completed volunteer forms are due April 17.
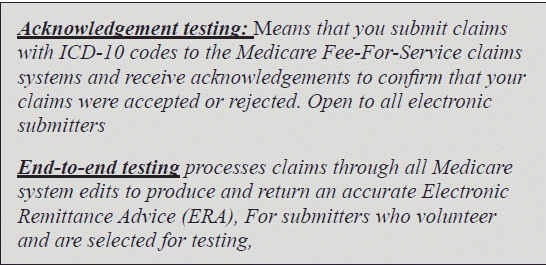
In addition to this, providers are invited to submit acknowledgement testing claims at any time up until the deadline of Oct. 1 of this year. The advantage to testing during the testing week allows for additional customer service support from the MAC and during this time CMS collects data so CMS can report the national statistics.
Each MAC will select 50 participants per testing round. To be eligible to test, you must be ready for ICD-10, including ensuring that your vendor software is ready to use. In addition, you must be a direct submitter to Medicare and be able to receive electronic remittance advice.
If you get selected, you’ll need the ability to submit 50 claims to a particular Medicare Administrative Contractor (MAC); you must provide the MAC:
You may use these in any combination on the 50 claims. Use the same HICN on multiple claims.
Point to consider: The MAC will copy production information into the test region for the HICNs that you provide.
What to Know During Testing
Once you are selected for end-to-end testing, you are automatically registered for the later rounds of testing so you need not reapply. Moreover, a new group will be selected for each testing period, and these groups will be able to test in addition to the already chosen testers.
PHI in safe hands: CMS assures that using real data for this test does not cause any additional risk of release of PHI, because the test claims would be accepted into the system using the same secure method used for production claims on a daily basis. They will be processed by the same MACs who process production claims, and all the same security protocols will be followed.
“What CMS is doing is to use existing processes and thus the security for these processes should be sufficient,” says Duane C. Abbey, PhD, president of Abbey and Abbey Consultants Inc., in Ames, IA.
Discern the dates of service: The MACs will accept the claims with an ICD-10 code as per the following rule:
Failed claims: Institutional claims that fail do count toward the 50 claim submission limit. If claims accepted by the front end edits do not appear on the remittance advice, please contact the Medicare Administrative Contractor (MAC) for further information.
However, claims that are rejected by front end editing do not count toward the 50 claim submission limit; therefore, they should be corrected and resubmitted.
Claim with a future date? You can send the Inpatient Rehabilitation Facility (IRF) claim with a valid Case-Mix Group (CMG) code on the claim and a Skilled Nursing Facility (SNF) claim with a valid Resource Utilization Group (RUG) code on the claim, with the date of service in the future. For testing purposes, only a claim with a valid Health Insurance Prospective Payment System (HIPPS) code will be required. You do not need to submit the supporting data sheets.
Resource:You can read more about ICD-10 testing opportunities at www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/Downloads/SE1435.pdf.