ICD 10 Coding Alert
Will Your ICD-10 Claims Be Accepted After Grace Period Ends?
If your ICD-10 denials are low and your coding confidence is high, you could have a false sense of security—and that could be going away in just a few months.
Here’s why: Nearly a year ago, CMS announced that it would implement a grace period for the ICD-10 rollout, assuring practices that MACs would not deny claims with the wrong ICD-10 codes, as long as the codes were from the right “family.” Although this announcement gave practices a temporary reprieve on the ICD-10 denials they were anticipating as of Oct. 1, 2015, that reprieve is about to expire, so now is the time to ensure that your ICD-10 codes are as accurate as possible.
The grace period ends on Sept. 30, and there’s a strong chance that denials will increase thereafter, says Monica Smith, RHIT, CPC, CRCR, an associate in Kraft Healthcare Consulting’s compliance services division and an ICD-10 trainer. “Physician offices aren’t used to the specificity that is required for ICD-10.”
You’ve now got four months to re-invigorate your ICD-10 training and maintenance programs before the grace period ends. The following tips will help ensure that you’re on the right track to successfully collect for your services.
Don’t Be Vague
If you haven’t yet brushed up on ICD-10’s specificity requirements, now is the time. “Physicians need to state the diagnosis as specifically as they can, being sure to link conditions if needed,” Smith advises. “If the conditions are specific, then the other issues will not be a problem.”
For example, simply documenting “distal radial fracture” may not be sufficient, Smith says. “Different types of fractures are able to be specified, such as Colles’, Smith’s, Barton’s, torus, etc.”
In addition, Smith advises, always link conditions if applicable. “Be specific, document it – if it’s not written, it can’t be coded.” In addition, she advises practices to review the updates every Oct. 1 so you don’t miss any new, revised or deleted codes.
List All Treated Diagnoses
When assigning ICD-10 codes, you should first code the main or most serious diagnosis, which is typically determined as follows:
After the primary diagnosis, you’ll then list additional diagnoses describing other conditions that the patient has as well. “Code all documented conditions that coexist at the time of the encounter/visit, and require or affect patient care treatment or management,” the ICD-10 manual states. “Do not code conditions that were previously treated and no longer exist. However, history codes (Z80-Z87) may be used as secondary codes if the historical condition or family history has an impact on current care or influences treatment.”
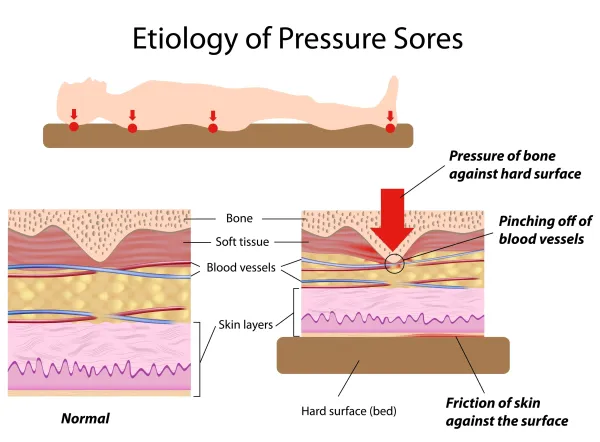
Example: Suppose your patient has a stage 3 pressure ulcer on her right buttock and a stage 4 pressure ulcer on her right shoulder blade. She also has a deep tissue injury (DTI) on her right heel. She has type 2 diabetes and failure to thrive. You will be providing dressing changes on the stage 3 and stage 4 pressure ulcers and pressure relief for her DTI with no dressings. Code for this patient with the following ICD-10 codes:
First, list your patient’s pressure ulcers, since they are the focus of care. Sequence the stage 4 pressure ulcer first (L89.114) followed by the stage 3 (L89.313).
Next, list your patient’s diabetes. Her pressure ulcers aren’t a result of the diabetes, so there is no need to use manifestation coding here. Instead, list E11.9 to indicate your patient’s type 2 diabetes.
Follow the diabetes code with R62.7 to indicate that your patient has adult failure to thrive. Then, list L89.610, the unstageable pressure ulcer code, to indicate that the patient also has a DTI.
Finally, report Z48.00 to indicate that you will be providing dressing changes. To find this code in the Alphabetic Index of your ICD-10 manual, look under “Aftercare, Involving, Removal of” or “Change, dressing (nonsurgical)” or “Admission, Removal of” or “Removal (of).”
Related Articles
ICD 10 Coding Alert
- News You Can Use:
Will Your ICD-10 Claims Be Accepted After Grace Period Ends?
Don’t forget: MACs are still going easy on denials. If your ICD-10 denials are low [...] - Gastroenterology:
Size Up These 7 Gastroenterology Changes Planned for ICD-10-CM 2017
Get ready for more specific pancreatitis codes. The CDC has posted a preliminary list of [...] - Dermatology:
Look for New Hematoma, Redundant Skin Dx Codes
Proposed list would introduce nearly 2,000 new codes, effective Oct. 1. Six months after ICD-10 [...] - General Surgery:
Get Ready for Dx Updates This October
Cardiovascular system changes and more will impact your practice. After a five-year code freeze to [...] - Oncology & Hematology:
Pick Up Cues From Changes Proposed For Upcoming Annual Update In ICD-10-CM
Prepare to implement revisions in your Hodgkin lymphoma diagnosis coding. The CDC has posted a [...]