Eli's Hospice Insider
New Hospice Payment Reform Model Hits Jan. 1
Hospices will see 1.1% pay increase overall.
In the New Year, figuring out how many days your patients have received hospice services — from anyone — will be crucial to your bottom line.
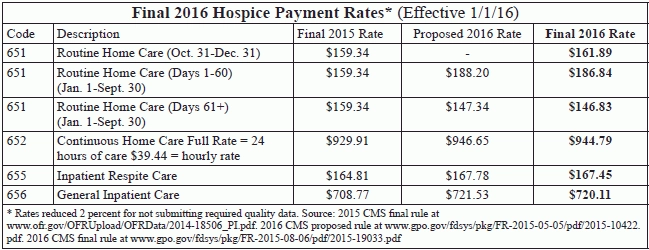
In the final rule for hospices’ 2016 payment, the Centers for Medicare & Medicaid Services finalizes its proposal to split hospices’ routine home care rates into two tiers: higher payment for RHC days 1-60, and lower payment for RHC days 61 and higher (see chart p. 67 for rates). Until the tiered model takes effect in January, hospices will see an updated RHC payment rate.
Remember: Sequestration will almost certainly continue to take a 2 percent bite out of these rates, notes Theresa Forster with the National Association for Home Care & Hospice. “We do anticipate a continuing drag from the sequester” for years to come, Forster tells Eli.
When CMS issued the proposed tier model, some hospices were surprised that the agency didn’t try to implement a more complex methodology (see Eli’s Hospice Insider, Vol. 8, No. 6). In the rule published in the Aug. 6 Federal Register, CMS responds to a number of provider comments about the system.
For example: Some commenters asked for higher RHC rates through day 90. “We concur with [the Medicare Payment Advisory Commission’s] comments on the proposed rule cautioning against any changes to the proposed structure that would lengthen the period for the initial payment rate … because that would result in a lower initial payment rate and represent a smaller increase in reimbursement for shorter stays,” CMS responds.
Likewise, CMS also rebuffed suggestions to shorten the time period for the higher RHC rate. “Visit intensity declines after 7 days of hospice care until day 60 of hospice care when the visit intensity becomes flat throughout the remainder of the hospice episode (excluding the last 7 days prior to death),” the agency explains in the rule. “It is for this reason that we proposed to pay a higher rate for the first 60 days and a lower rate thereafter.”
“CMS did consider establishing an even higher rate for the first 7 days of care,” the agency adds. However, given concerns voiced by the industry and MedPAC “that short lengths of stay may prevent patients and family caregivers from benefiting fully from the range of specialized services and compassionate care that hospices offer, we decided to propose a higher RHC rate for days 1-60 and a lower RHC rate for days 61 and beyond as to not provide a larger incentive for hospices to target short stay patients.”
No Billing Changes Required
CMS was more receptive to requests to delay the implementation date for the new system. On one hand, Medicare has been prepping its systems already. “We do not have concerns about the readiness of Medicare systems on October 1, 2015,” CMS says in the rule. And hospice billing won’t require any big changes, because the payment levels will be determined by the Medicare claims system. Thus, “systems for submitting claims and receiving Medicare payment should not be affected and the need for retraining billing staff should be limited,” CMS believes. “But hospices may need to change their internal accounting systems,” the agency allows.
On the other hand, “while CMS is ready ... we anticipate that state Medicaid agencies may encounter difficulties in making the necessary systems and software changes to be ready to implement the proposed RHC rates on October 1,” CMS says. “Therefore, we will delay implementation of both the proposed RHC rates and the SIA payment until January 1, 2016 in order to ensure, to the greatest extent possible, that the state Medicaid agencies can likewise implement these changes.”
Doubtful: Even that timeframe may not be enough for Medicaid. “Medicaid programs will need to make major adaptations and they have had very limited warning,” Forster notes. “CMS has had an ongoing sense of what they planned to do and so could make systems changes throughout this past year, but Medicaid programs have not.”
“We are most concerned about state Medicaid agencies and their ability to get systems in place in time for a January 1 implementation,” says Judi Lund Person with the National Hospice & Palliative Care Organization.
The delay to allow Medicaid to get up to speed will also give hospice vendors time to catch up to the system as well, Forster hopes.
Major Challenges Ahead
Under the new system, “hospices are concerned about the challenges in predicting with accuracy whether the reimbursement for a day of care will be at the higher or lower tier payment,” Lund Person relates. The information available in the Medicare system will only be as current as the claims hospices are submitting.
Thanks to the tier uncertainty and not being able to know how much, if any, Service Intensity Add-on (SIA) services will be furnished. “One of the biggest challenges for hospices will be anticipating the financial impact on their programs,” Forster says. “There are many more factors that can have an impact on their bottom line than previously.”
Buckle up: This reform is just the beginning, CMS says in the rule. “The RHC rates … and SIA payment will advance hospice payment reform incrementally … while simultaneously maintaining flexibility for future refinements,” CMS notes.
“CMS hopes to advance hospice payment changes over time,” the agency says in the rule.
Future reform will be data-driven, CMS says in the rule. Data from recent hospice claim and cost report revisions should “provide more comprehensive information on the costs associated with the services provided by hospices to Medicare beneficiaries by level of care,” CMS notes.
And enhanced diagnosis code reporting on claims, required in this rule, will further inform payment reform, CMS says.
Note: See the rule at www.gpo.gov/fdsys/pkg/FR-2015-08-06/pdf/2015-19033.pdf.
Eli's Hospice Insider
- Reimbursement:
New Hospice Payment Reform Model Hits Jan. 1
Hospices will see 1.1% pay increase overall. In the New Year, figuring out how many [...] - Payment:
CMS Relents So SIA Will Apply To Nursing Home Residents Too
Prepare to change how you bill nursing visits. Your nursing home patients won’t count against [...] - Reimbursement:
Above-Cap Hospices Fare Worst Under New System
Whether your Medicare reimbursement goes up or down under the new rule depends on your [...] - Finance:
Hospice Providers Will Be Happy To Say Good-Bye To BNAF Cuts
Plus: Prepare for CBSA transition. Seven years of Budget Neutrality Adjustment Factor reductions to Medicare [...] - Regulations:
More Hospices Likely To Exceed Caps Under New Rule
Change to slice half a billion dollars from reimbursement. The Centers for Medicare & Medicaid [...] - Diagnosis Coding:
Get Ready To Shoulder A Drastically Expanded Diagnosis Coding Burden
Hospices have to take on increased coding and ICD-10 almost simultaneously. New diagnosis coding instructions [...] - Hospice Item Set:
New 30-Day HIS Submission Deadline Starts In January
You’ll lose out on payment if you don’t meet the threshold. Nearly a quarter of [...] - Hospice News:
Beware New Hospice Denial Codes Indicating NOE-Delaying ICD-9, ICD-10 Problems
Get to know three new reason codes that will point the way to diagnosis coding [...]

