Eli's Hospice Insider
Medicare Payment Rates To Inch Up 1% In 2014 -- Before Sequestration
More payment changes are on the way, CMS signals in final rule.
Your costs are likely to go up next year, but your hospice reimbursement rates probably won’t.
That’s because the Centers for Medicare & Medicaid Services has finalized a 2014 payment rule that includes a mere 1 percent increase in Medicare hospice rates. And a 2 percent reduction due to sequestration is likely to wipe out even that modest update.
The increase is down slightly from the proposed rule CMS issued in May (see Eli’s Hospice Insider, Vol. 6, No. 6). That’s due to a slightly larger productivity adjustment (0.5 instead of 0.4 percent). CMS arrives at the final increase by subtracting the productivity adjustment and an Affordable Care Act-mandated 0.3 percent reduction from the 2.5 percent inpatient hospital market basket update, according to CMS’s final rule published in the Aug. 7 Federal Register.
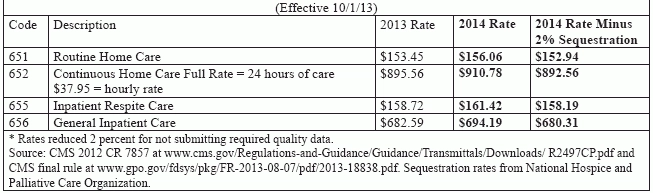
As of Oct. 1, CMS will increase the four hospice per diem rates by 1.7 percent, (see chart, on page 75, for new rates). But a Budget Neutrality Adjustment Factor reduction and other wage index changes will bring the overall reimbursement change to 1.0 percent.
This is the fifth of seven years phasing out the BNAF. CMS phased out 10 percent of the BNAF in 2010, 15 percent in 2011 and 2012, and will phase out additional 15 percent increments through 2016.
Routine Home Care, Nursing Home Changes Ahead
CMS once again discusses the concept of reducing the routine home care (RHC) rate. “As we continue to gather and analyze more data for payment reform, we have found evidence of a potential misalignment between the current RHC payment rate and the cost of providing RHC,” CMS says in the rule. “One potential option to address this misalignment could be to rebase the hospice RHC rate.”
As in the proposed rule, CMS also reiterates the possibility of reducing payment rates for patients in nursing homes. In analyzing visit data, CMS found “significantly more aide services were provided to NF/SNF patients than to patients at home, even after controlling for patient and provider characteristics,” the agency notes.
But CMS makes no proposals in the final rule on either of these issues. Stay tuned for developments on this front, experts say. Any savings from either of these changes would be redistributed to other areas in a budget neutral manner, the agency notes.
Tough road ahead: The 2014 payment rule is full of big changes for hospices, notes Judi Lund Person with the National Hospice & Palliative Care Organization (see stories, p. 75 and p. 77, for coverage of other major provisions in the rule). “There is a great deal of regulatory activity for hospices, and the hospice community is addressing many different issues at the same time in aiming for compliance,” Person tells Eli. “It will be a very daunting task over the next 18 months to 2 years.”
Note: The final rule is at www.gpo.gov/fdsys/pkg/FR-2013-08-07/pdf/2013-18838.pdf.
Eli's Hospice Insider
- Reimbursement:
Medicare Payment Rates To Inch Up 1% In 2014 -- Before Sequestration
More payment changes are on the way, CMS signals in final rule. Your costs are [...] - Payment:
Check Out Your New Hospice Wage Index
Plus: Cap amount for 2014 released. The annual wage index gamble for hospices has wrapped [...] - Diagnosis Coding:
Medicare System To Kick Back Failure To Thrive, Debility Claims Beginning In Fall 2014
Code all coexisting conditions, CMS also urges in final rule. You’ve got about a year [...] - Regulations:
Get Ready To Report This New Data Set Next Summer
Gear up now for the July 1 start date for HIS. Get ready to fill [...] - Referrals:
Scrutiny May Squeeze Referrals
Billing report contractor, ZPIC contact docs about home care and hospice referrals. Reviewers peering over [...] - Hospice News:
Surveys To Happen More Often If OIG Gets Its Way
Hospice goes 22 years with no surveys. Does getting surveyed about once a decade sound [...] - Hospice News:
Hospice Spending Slows, CBO Says
The meteoric rise of hospice spending seems to have come to an end. Medicare hospice [...] - Hospice News:
Drug Reporting May Weigh Heavily On Hospices
Hospices should get ready for a heavy reporting burden next year. In July, CMS released [...] - Hospice News:
NIH-Funded Study Evaluates Palliative Home Care For HIV Patients
A $1.7 million study will examine the effect of home health visits on a less [...]

