No payment reform yet, but it’s on the horizon.
Hospices’ financial burden will increase as Medicare tries to shift more costs onto their plates in the newest proposed payment rule, but they will have a little more cash to deal with it.
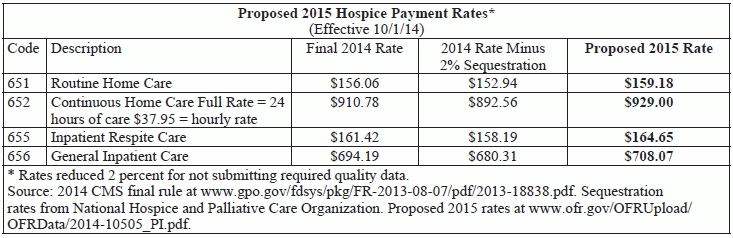
In its proposed rule for hospice payment in 2015, the Centers for Medicare & Medicaid Services floats a 1.3 percent payment increase to hospice reimbursement rates (see rates, p. 45). The figure derives from a 2.7 percent inflation update, minus 0.7 percent for reductions mandated by the Affordable Care Act, and minus another 0.7 percent due to updated wage data and the sixth year of CMS’s seven-year phase-out of its wage index budget neutrality adjustment factor (BNAF).
Watch out: The increase could be wiped out by the 2 percent sequestration reduction, which is not included in the calculation.
CMS proposes a hospice aggregate cap for the fiscal year ending Oct. 1, 2014 of $26,725.79, up from $26,157.50 for the current year. And as always, Medicare hospice inpatient stays in excess of 20 percent of total Medicare hospice days are to be reimbursed at the routine homecare rate, CMS notes.
Cap calculation methodology is the same, but CMS is calling for a major change in how hospices that exceed their cap handle the overpayments.
Current way: “Medicare contractors complete the hospice cap determination approximately twelve to eighteen months after the cap year in order to demand any overpayments from the hospices,” CMS notes.
New way: CMS wants “hospices to calculate their inpatient and aggregate caps five months after the cap year and remit any overpayment,” the rule says. That’s similar to the cost report timeline, the agency adds. Even though the cap determination is not actually tied to the cost report, “requiring hospices to complete a cap determination and remit any overpayment is consistent with what is currently required of all other provider types that file a Medicare cost report.” the rule says.
CMS estimates “that it would take a hospice about 1.5 hours to complete its cap determination,” it says in the rule. “All information needed to file the cap determination is available in the Provider Statistical and Reimbursement (PS&R) system.”
Consequence: “If a hospice does not complete its cap determination timely, its Medicare payments would be suspended until the cap determination is complete and received by the contractor,” CMS warns in a release. “To better safeguard the Medicare Trust Fund, we believe that demands for cap overpayments should occur sooner” than they currently do.
Your Claims Data Will Shape Pay Reform
CMS is holding off on proposing payment reform for a second year, while it compiles and analyzes more data. “We recently required additional information on hospice claims regarding drugs and certain durable medical equipment, effective April 1, 2014; and are in the process of finalizing changes to the hospice cost report to better collect data on the costs of providing hospice care,” CMS says in the rule. The stats cover hot button topics like live discharges, skilled services directly before death, inpatient and continuous care, and non-hospice spending for hospice patients.
“The additional information on hospice claims and the hospice cost report will be used in our hospice payment reform efforts, once the data are available for analysis,” CMS says.
Congress gave CMS permission to implement hospice payment reform as early as October 2013, but the agency has been cautious in moving toward the goal. Policymakers want more data before moving ahead.
Meanwhile, the Medicare Payment Advisory Commission has been calling for a U-shaped payment model with higher payments at the beginning and end of care and lower payments in between for longer stays. Medicare officials are considering a J-shaped model as well, with somewhat higher payments at the start, lower payments in the middle, and significantly higher payments at end of life.