CMS may cut how much you get paid for Routine Home Care.
BNAF and Affordable Care Act reductions are taking their toll on hospices’ Medicare payment rates for 2014.
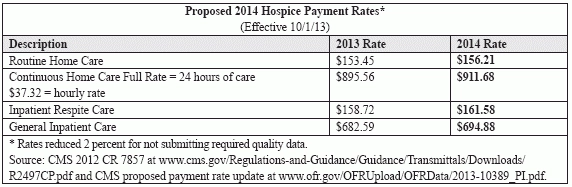
In a proposed rule published in the May 10 Federal Register, the Centers for Medicare & Medicaid Services sets a 1.1 percent payment rate increase for hospices. CMS will increase the four hospice per diem rates by 1.8 percent, the agency proposes (see chart, p. 43, for new rates). But a Budget Neutrality Adjustment Factor reduction and other wage index changes will bring the overall reimbursement change to 1.1 percent, CMS explains in the rule.
Change: CMS is now publishing stand-alone proposed rules on hospice rates instead of just rate notices or changes proposed in the home health prospective payment system rule, notes the National Hospice and Palliative Care Organization.
BNAF Phase-Out Nearing Completion
This is the fifth of seven years phasing out the BNAF. CMS phased out 10 percent of the BNAF in 2010, 15 percent in 2011 and 2012, and will phase out additional 15 percent increments through 2016.
The inflation update actually starts as 2.5 percent, but the ACA reductions include a 0.4 percent productivity adjustment and a 0.3 percent inflation adjustment, CMS says in the rule.
Like the Medicare Payment Advisory Commission and the HHS Office of Inspector General, CMS notes the explosive growth of the hospice benefit in the last decade. “The number of Medicare beneficiaries receiving hospice services has grown from 513,000 in FY 2000 to over 1.3 million in FY 2012,” CMS points out. “Similarly, Medicare hospice expenditures have risen from $2.9 billion in FY 2000 to $14.7 billion in FY 2012.”
CMS’s Office of the Actuary expects Medicare hospice spending to grow about 8 percent annually in the future, the rule says.
Urban hospices in New England (CT, ME, MA, NH, RI, VT) will see the biggest pay bump due to the rule at 2.2 percent, predicts CMS in its impact analysis. Urban hospices in the Mountain region (AZ, CO, ID, MT, NV, NM, UT, WY) would see the smallest increase at 0.4 percent.
For rural hospices, providers in East South Central (AL, KY, MS, TN) and Outlying (Guam, PR, Virgin Islands) regions would see a 1.8 percent increase, while those in the Pacific (AK, CA, HI, OR, WA) region would actually see a 1.1 percent decrease, CMS forecasts.
You May Get Too Much For Routine Home Care, CMS Says
Medicare may be paying too much for routine home care, CMS also says in the rule. “It is CMS’ intent to ensure that reimbursement rates under the Hospice benefit align as closely as possible with the average costs hospices incur when efficiently providing covered services to beneficiaries,” the rule says. “As we continue to gather and analyze more data for payment reform, we have found evidence of a potential misalignment between the current RHC payment rate and the cost of providing RHC.”
CMS uses nine components to figure RHC rates: nursing care; home health aide; social services/therapy; home respite; interdisciplinary group; drugs; supplies; equipment; and outpatient hospital therapies. “At this time, we do not have the data to support rebasing six of the nine cost components,” CMS admits. “Information on the utilization of drugs, supplies, and equipment is not available from hospice claims data, and the corresponding information that is available from cost reports, such as outpatient hospital therapies, is not sufficiently detailed to allow for rebasing.”
But CMS does have info on the three clinical components (nursing, aide, and social services/ therapy) that make up 70 percent of the RHC rate. It may rebase that segment of the rate based on those components, the agency suggests. More information on the possibility is in a study by contractor Abt Associates.
The rule addresses a host of hospice issues in addition to 2014 payment rates. They include:
· Payment reform. CMS sets no firm timeline for payment reform, but does update hospices on its work in the area and possible changes in store.
Plus: Although not included in this rule, CMS did issue proposed cost report changes in a separate Paperwork Reduction Act notice at www.cms.gov/Regulations-and-Guidance/Legislation/PaperworkReductionActof1995/PRA-Listing.html — scroll down to the “Hospice Cost and Data Report” listing on April 29. Improved cost report data would contribute to payment reform, industry observers expect.
· Nursing home residents. As part of payment reform, CMS is considering reducing payment rates for hospice patients in nursing homes. “Hospice patients in a NF/SNF receive more visits than patients at home, though the length of those visits is shorter,” CMS discovered in analysis of claims data. “Given the presence of the paid caregiver in the NF/SNF, we would expect that on average, there would be fewer hospice aide services provided to hospice patients in a NF/SNF than to hospice patients at home.”
· Quality reporting. CMS wants to ax the current two quality measures hospices are reporting and instead use a seven-item Hospice Item Set (HIS), according to the rule. “Hospices would be required to complete the HIS at admission and discharge on all patients admitted to hospice starting July 1, 2014,” CMS notes in a fact sheet about the rule. “HIS data submission would affect the payment determination for FY 2016.”
Hospices would have to complete a HIS data set for every patient, regardless of payor source, stresses the National Association for Home Care & Hospice.
· Patient satisfaction survey. CMS wants to use a Hospice Experience of Care survey starting in 2015, it says. The survey would be for patients’ informal caregivers and would address “hospice provider communications with patients and families; hospice provider care, and overall rating of hospice,” CMS notes in the fact sheet. Survey participation would be part of quality reporting and affect reimbursement starting in 2017, CMS proposes.
Note: A link to the proposed rule and wage index notice is in the “Spotlights” box at www.cms.gov/Center/Provider-Type/Hospice-Center.html. Comments on the rule are due June 28.
The Abt study is at www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/Hospice/Downloads/Hospice-Study-Technical-Report-4-29-13.pdf .