Home Health Coding and OASIS Expert
Say Goodbye to 200 Case Mix Diagnoses in 2015
Two OASIS items also lose their scoring impact.
Your case mix diagnoses list has been getting shorter each year. The Centers for Medicare & Medicaid Services removed 170 codes in 2014, and the 2015 home health prospective payment system strips case mix points from about 200 diagnosis codes.
CMS also dropped case mix points from two OASIS items. These changes are part of a move to align payments “with current utilization data in a budget neutral manner,” the agency explained in the 2015 HH PPS final rule.
Warning: This case mix recalibration could take a big bite out of your budget if your patients fall into the categories losing reimbursement under the new model. “It is really going to be a tough year for HHAs,” predicts Judy Adams with Adams Home Care Consulting in Asheville, N.C.
“You can count all the blindness/low vision, pulmonary and psych codes gone,” says Lisa Selman-Holman, JD, BSN, RN, HCS-D, COS-C, HCS-O, consultant and principal of Selman-Holman & Associates and CoDR — Coding Done Right in Denton, Texas. “CMS did not issue a new list of case mix codes to replace the one we’ve had. They simply removed the points from those rows in the case mix variable table. You’ll have to update your own list by blocking them out of the list in your coding manual.”
CMS made “significant changes to the point values for the variables in the four-equation model” under PPS. “These reflect changes in the relationship between the grouper variables and resource use since 2005,” CMS said in the rule. These changes include “the removal of case mix points for a number of interactions, primary GI diagnosis, etc.,” Adams said.
Plus: 2015 brings big changes for diabetes, long one of the most impactful case mix diagnoses for home health. A primary diagnosis of diabetes will no longer gain any points in an early or late episode with low therapy. And you’ll only earn one point for a diabetes diagnosis in an early episode with low therapy. In the other three equations, when diabetes is a secondary diagnosis, you won’t earn a single point for this diagnosis.
Two OASIS items have also lost their case mix points. Items M1200 — Vision and M2030 — Injectable drug use will no longer impact HHRG. CMS reports that documentation didn’t support the need for increased resources in relation to scores for these two items.
The case mix change will have a tremendous impact on agencies, predicts Arlene Maxim, RN, founder of A.D. Maxim Consulting, A.D. Maxim Seminars, and The National Coding Center, in Troy, Mich. And many agencies aren’t even aware of these changes, she says.
Agencies will feel the sting most for those patients with the highest rate of rehospitalization — those with congestive heart failure, chronic obstructive pulmonary disease and diabetes, Maxim predicts. “Agencies are going to have to take a look at the types of patients they have been admitting over the past 12 months or so and analyze the impact,” she says.
Do this: To survive these cuts, agencies will need to carefully watch every single referral they receive, budget every single case, and focus on the number of visits and types of disciplines they offer, Maxim advises. “This is going to be a big financial hit to homecare companies all across the U.S.,” she predicts.
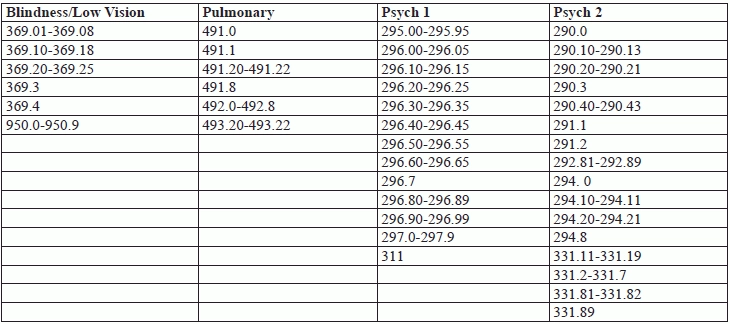
Source: Oct 2014 HHPPS Grouper Software and Jan 2015 HHPPS Grouper Software available here: www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HomeHealthPPS/CaseMixGrouperSoftware.html
Warning: CMS has piled the points into equations 2 and 4, those equations indicating 14 or more therapy visits, says Selman-Holman. “However, CMS has made it clear that they’ll be watching for increased therapy utilization. Some agencies will be tempted to increase the number of therapy visits in order to garner more clinical points. Always make therapy visit decisions based on medical necessity.”
Home Health Coding and OASIS Expert
- Diagnosis Coding:
Clinicians: Don't Miss this Coding Detail in the Updated OASIS Guidance Manual
It’s time to take a look at your coding policy. While the OASIS-C1 was originally [...] - Diagnosis Coding:
Beware Increased Emphasis on Clinician Sequencing
Accurate coding takes more than just looking up a code in a book. Overall, there [...] - Policies:
Include 5 Key Components For a Successful Coding Policy
Don’t overlook your correction process. Your agency’s ICD-9 coding policy ensures accuracy, consistency, and compliance [...] - Follow This Proven Sequencing Method
As a clinician, how do you determine the primary and secondary diagnoses? Make certain you’re [...] - Face-To-Face:
Will Your F2F Burden Grow in 2015?
Good news: New F2F documentation doesn’t always require a new F2F visit. The 2015 home [...] - ICD-10:
Full Steam Ahead for ICD-10
Take a 3-pronged approach to gearing up for transition day. The Oct. 1 ICD-10 implementation [...] - Conquering Case Mix:
Say Goodbye to 200 Case Mix Diagnoses in 2015
Two OASIS items also lose their scoring impact. Your case mix diagnoses list has been [...]

