VBP Ground Continues To Shift Under HHAs’ Feet, Experts Say
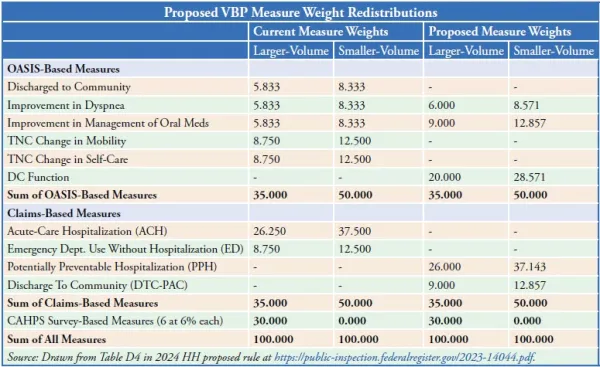
Under newly proposed configuration, half of VBP points will come from only 2 measures. As home health agencies navigate through their first year of the Expanded Home Health Value-Based Purchasing program, Medicare is proposing to change the rules of the game. The Centers for Medicare & Medicaid Services wants to swap out the quality measures used to generate HHAs’ VBP scores and reweight them, which could mean things you’ve targeted for quality improvement could become moot. In its 2024 home health proposed rule, CMS proposes to make these changes effective Jan. 1, 2025: In other words, CMS wants to remove five measures and replace them with three measures, and then reweight them, the rule summarizes (see chart, p. 191, for reweighting). Why make these big changes just as HHAs are getting going? “The proposed changes will align the measures used in the expanded HHVBP Model with the measures in the HH QRP and publicly reported on Home Health Care Compare. This alignment will support comparisons of provider quality and streamline home health providers’ data capture and reporting processes,” CMS says in the rule. The claims-based DTC-PAC measure also “assesses broader outcomes by assessing post-discharge hospitalization and mortality. Specifically, it first examines whether a patient was discharged to the community from the PAC setting. For patients discharged to the community, this measure examines whether they remained alive in the community without an unplanned admission to an acute care hospital or LTCH in the 31-day post-discharge observation window following discharge to the community,” CMS praises. But CMS’ claim of QRP alignment doesn’t hold for the DC Function measure, which is only proposed for QRP inclusion starting in 2025 (see related story, p. 192). CMS has a preemptive response for that. “While the DC Function measure is not yet implemented in the HH QRP or other PAC programs, the OASIS data elements used to calculate this measure have been collected since 2019. As such, we believe HHAs have had sufficient time to ensure successful reporting of the data elements needed for this measure,” the rule argues. CMS also praises the DC Function measure because it “addresses self-care and mobility through a single measure rather than two measures, thereby streamlining the calculation and reporting of measure results.” On the other hand, the PPH measure has been in the works for a while and is scheduled to go live on Home Health Care Compare later this month (see HHHW by AAPC, Vol. XXXII, No. 13). “Replacing ACH and ED Use with PPH would further align the expanded Model’s applicable measure set with the HH QRP measures,” CMS notes in the rule. The five CAHPS-based measures will remain the same under VBP. CMS also wants to reweight the measures once they are in place (see chart, p. 191). And the agency suggests rebasing the model year yet one more time, moving it to 2023 for the performance year starting 2025. Background: CMS originally set the baseline year at 2019, then last year moved it to 2022 over much industry protest via rule comment letters and other avenues. “If we finalize our proposal to use CY 2023 for the Model baseline year, we would provide HHAs with the final achievement thresholds and benchmarks in the July 2024 Interim Performance Report (IPR),” CMS offers. “For all measures but the claims-based DTC-PAC measure, this timeline allows for one year of performance between the first performance year and the proposed updated Model baseline year.” The DTC-PAC measure is an exception because it is based on two years’ of data. CMS considered delaying implementation of the new measures in a variety of configurations, the rule discussion reveals. But “we prefer the proposed timeline … because it expedites alignment with the HH QRP, SNF VBP, and the other PAC programs and the timing corresponds with the proposed removal and replacement of other measures in the Model,” it says. Expect VBP Penalties To Exacerbate Access Problems The clutch of changes CMS is considering for VBP just as it’s getting off the ground “makes it extremely difficult to lay a foundation for success, particularly in something that is so new and even more so for providers that were not part of the original demonstration,” critiques consultant Angela Huff with FORVIS in Springfield, Mo. “The VBP race … is underway and halfway through in this first year of expanded demonstration,” Huff emphasizes. “Agencies are still trying to navigate these changes in their organizations and haven’t even had a full year yet to navigate this new program only to get news that the rules of the race are going to be shifting again,” she tells AAPC. “The proposed reduction in VBP from 12 to 10 performance measures and the resulting redistribution of the weighting of those measures means that nearly 50 percent of the possible VBP points will come from only two measures: discharge function and potentially preventable hospitalization,” points out reimbursement expert M. Aaron Little with FORVIS. “The uneven weighting across the 10 measures will no doubt create real challenges for many agencies,” Little predicts. The change “clearly demonstrates CMS’ intentions to align VBP with QRP while incentivizing practices to reduce preventable hospitalizations,” Little tells AAPC. That’s no surprise, given that CMS highlights in the rule that the model’s “overall economic impact … for CYs 2024 through 2027 is an estimated $3.376 billion in total savings to FFS Medicare from a reduction in unnecessary hospitalizations and SNF usage as a result of greater quality improvements in the HH industry.” That savings comes at nearly no cost to HHAs, CMS implies in the regulation. “No aggregate increases or decreases [are] expected to be applied to the HHAs competing in the expanded Model,” it says. That may be true on average, but “VBP is going to result in further reductions in reimbursement for some providers, which will only compound the effects we are already seeing in the industry,” Huff warns. “All of this leads to impacts to patient care that are likely not going to be positive,” she adds. CMS isn’t done tinkering with the model, either. “While we are not making any specific proposals here, we invite stakeholders to suggest future measures and the value they may provide to the expanded HHVBP Model,” CMS says in the rule. Kick VBP Appeals Up Another Level Don’t miss: CMS also proposes some structural changes to the VBP appeal process. The changes would basically give HHAs an extra appeal step in the process. Currently, HHAs can ask for a recalculation of their Total Performance Score (TPS) and then request a reconsideration of those results, if desired. Under the proposal, “an HHA may request [CMS] Administrator review of a reconsideration decision within 7 days from CMS’ notification to the HHA contact of the outcome of the reconsideration request,” the rule says. “This proposed change would ensure that accountability for the decisions of CMS is vested in a principal officer and brings the reconsideration review process to a more similar posture as other CMS appeals entities that provide Administrator review.”