Take A Closer Look At TPS Before Value-Based Purchasing Pay Adjustments Begin
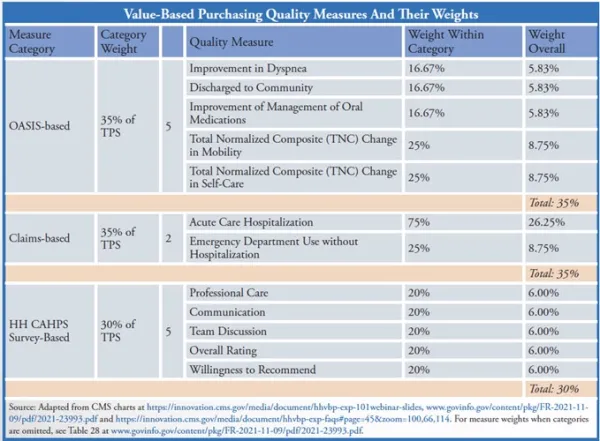
HHAs would like their own data ASAP — but it looks like they won’t get it any time soon. The implementation date for the Expanded Home Health Value-Based Purchasing payment model is rushing up. Make sure you understand one of its basic calculations — before your bottom line depends on it. Definition: Under VBP, “the Total Performance Score (TPS) is the numeric score awarded to each qualifying HHA based on the weighted sum of the performance scores for each applicable measure,” the Centers for Medicare & Medicaid Services explains in its Expanded Home Health VBP Model Frequently Asked Questions (FAQs) updated last month. “CMS determines the TPS by weighting and summing the higher of that HHA’s achievement or improvement score for each applicable measure. A qualifying HHA will receive a numeric score ranging from zero (0) to one hundred (100).” Five OASIS-based measures will count toward 35 percent of the TPS; two claims-based measures will count toward 35 percent; and five Home Health CAHPS Survey-based measures will count toward 30 percent, noted Elaine Gardner with CMS contractor OASIS Answers Inc. in the HHVBP Model Expansion 101 webinar CMS held in February. (For a list of each measure comprising the three categories and their relative weights, see chart, p. 132). However, if HHAs don’t have enough data for any of those three categories, then CMS will omit that category and the other two categories will count for 50 percent each, or the remaining one category will count for 100 percent. The minimum thresholds are 20 home health quality episodes for the OASIS-based measure category, 20 home health stays for the claims-based measure category, and 40 completed surveys for the HHCAHPS survey-based measure category, CMS explains in the 2022 home health final rule published in the Nov. 9, 2021 Federal Register. HHAs that want to know more about how their TPS is calculated may have to wait. “In addition to what’s included in the calendar year 2022 final rule, additional resources about the calculation of the total performance score and payment adjustments will be available during the calendar year 2022,” Gardner told agencies attending the February webinar. HHAs will get information about their TPS scores on a quarterly basis in Interim Performance Reports (IPRs), CMS noted in its HHVBP Newsletter for February. “The information in the IPR reflects calculation of the TPS based on quarterly data collection periods. CMS issues two versions of the IPR — a preliminary version and a final version,” according to the newsletter. The TPS score that CMS will use to adjust your payment rate will come in the Annual Total Performance Score & Payment Adjustment Reports (Annual Reports), CMS notes in the newsletter. “CMS issues three versions of the Annual Report — preview, preliminary, and final,” the newsletter notes. Even if you don’t have enough data for any or all of the categories, you will continue to get quarterly reports, CMS says in a newly released VBP educational document, How to use Existing Quality Assurance and Performance Improvement (QAPI) Processes to Support Improvement in the Expanded HHVBP Model. “An agency that does not meet the minimum threshold will still receive quarterly IPRs for applicable measures,” CMS says in the document. But you won’t get a TPS score. “If an HHA does not meet the minimum threshold data for each measure category … on five (5) or more applicable measures, the agency will not receive a TPS for the applicable performance year or be subject to a payment adjustment for the applicable payment year,” CMS explains in the document. Good news: You’ll be able to see a sample report before VBP’s first performance year starts in January. “CMS will provide sample performance feedback reports to HHAs via iQIES when administratively feasible and based on available data, for learning purposes only during the pre-implementation year,” CMS noted in its December 2021 HHVBP Newsletter. “The sample reports will include the same information as an Interim Performance Report (IPR) and an Annual Total Performance Score (TPS) and Payment Adjustment Report (Annual Report). Data included in each report will be based on the same scoring methodologies and other policies finalized in the CY 2022 Home Health Prospective Payment System (HH PPS) rule,” CMS explains. Bad news: “These reports are for learning purposes only, not actual HHA performance data, to help HHAs understand how CMS will assess HHA performance,” CMS elaborates in the FAQs. Experts agree that HHAs would very much like to have their own agency-specific data as soon as possible. It’s unclear why CMS can’t produce at least baseline year, agency-specific data somewhat soon, given that most agencies’ baseline is 2019. “Preparation now would be much more meaningful if all agencies could see their specific baseline year performance today as measured within their assigned cohort,” emphasizes reimbursement expert M. Aaron Little with BKD in Springfield, Missouri. v Note: Links to the rule, webinar, FAQs, HHVBP newsletters, and more are at CMS’ Expanded HHVBP Model webpage at https://innovation.cms.gov/innovation-models/expanded-home-health-value-based-purchasing-model — scroll to the bottom.