Hospice Final Rule Reduces Pay Update Slightly
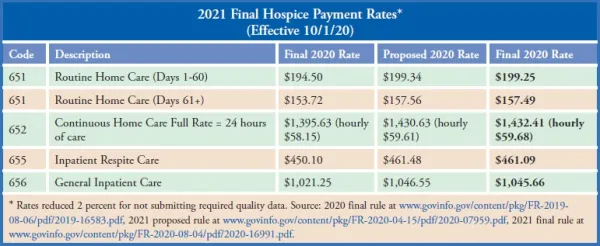
Big swings for wage index areas may batter already struggling hospices. A minor reduction in hospices’ inflation update will translate to $40 million less in hospice payments. Back in April, the Centers for Medicare & Medicaid Services proposed increasing hospice payment rates by 2.6 percent, boosting payments by an estimated $580 million. Now in its newly issued final rule, CMS puts the increase at 2.4 percent, resulting in an estimated $540 million pay bump. Why the change? The lower update “is primarily driven by slower anticipated compensation growth for both health-related and other occupations as labor markets are expected to be significantly impacted during the recession that started in February 2020 and throughout the anticipated recovery,” CMS explains in the rule published in the Aug. 4 Federal Register. The reduction is balanced out somewhat by CMS letting go of its idea to eliminate the service intensity add-on budget neutrality factor (SBNF). Then: “There have been very minor SBNF adjustments over the past several years suggesting that the utilization of the SIA from one year to the next remains relatively constant,” CMS explains. “Because the SBNF remains stable, we proposed to remove the factor to simplify the [Routine Home Care] payment rate updates.” However, commenters suggested a “significant increase” in the Continuous Home Care rate due to rebasing in 2020 “may incentivize an increase in visits made during the last 7 days of life,” and thus the SBNF should remain. Now: “After considering the comments … we are not finalizing the removal of the SBNF for FY 2021,” CMS concludes. “We agree that it is prudent to evaluate FY 2020 utilization data prior to eliminating the SBNF. We will continue to analyze data on visits in the last 7 days of life and whether there are changes in utilization that could affect overall budget neutrality.” The proposal may return, though. “If there continues to be very minor SBNF adjustments in the future, suggesting that the utilization of the SIA from one year to the next remains relatively constant, we may propose to remove the factor to simplify the RHC payment rate updates in future rulemaking,” CMS adds. In addition to retention of the SBNF, a “higher wage index standardization factor” than proposed also brings payment rates back up after the market basket decrease, NAHC notes. The final hospice cap amount for the FY 2021 cap year is $30,683.93, a 2.4 percent increase from this year, CMS notes in a fact sheet about the rule. (See chart, p. 236, for rates by care level.) Wage Index Changes Ahead CMS finalizes its proposal to implement the Office of Management and Budget’s wage index changes from 2018. The reorganization will flip some areas from rural to urban, urban to rural, or from one rural or urban area to another. (See more details about the change, which also affects home health agencies, in Eli’s HCW, Vol. XXIX, No. 25-26.) Medicare officials aim to mitigate negative changes by capping any decreases at 5 percent. CMS rejected a suggestion from the Medicare Payment Advisory Commission to cap decreases at 3 percent, calling the 5 percent figure “reasonable,” according to the rule. Note: A link to the wage index file is at www.cms.gov/medicaremedicare-fee-service-paymenthospicehospice-regulations-and-notices/cms-1733-f.