Home Health & Hospice Week
Hospice 2017 Pay Increase Improves Slightly To 2.1%
Pay raise will add an estimated $350 million to hospice payments next year.
If you were hoping to see some changes to Medicare’s 2017 proposed payment rule for hospices, prepare to be disappointed.
In the final rule released July 29, the Centers for Medicare & Medicaid Services adopts the policies largely as proposed back in April (see Eli’s HCW, Vol. XXV, No. 17). The final rule contains “no big surprises,” observes Theresa Forster with the National Association for Home Care & Hospice.
One welcome change, however, is a slight uptick in the payment increase that will begin Oct. 1.
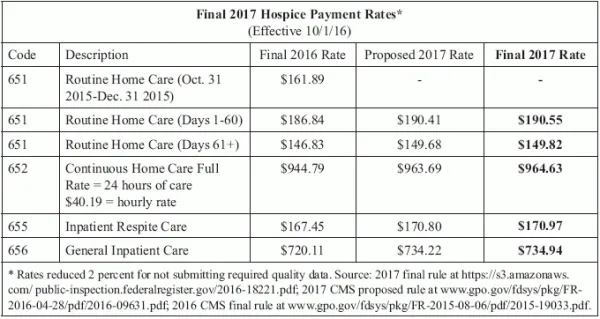
Breakdown: CMS will increase hospice payment rates by 2.1 percent in fiscal year 2017, a slight increase from the proposed 2.0 percent. The update reflects an estimated 2.7 percent inpatient inflation update, reduced by a 0.3 percent productivity adjustment and a 0.3 percent adjustment required by the Affordable Care Act, CMS notes in a release about the rule. (See specific service rates in chart, p. 223.)
Productivity factor reduced: CMS originally estimated a 2.8 percent inflation update reduced by a 0.5 percent productivity adjustment.
Thanks to the slightly increased update factor, the cap amount for 2017 will also be slightly higher than proposed — $28,404.99 instead of the $28,377.17 CMS originally floated.
CMS also forges ahead with its plan to change the cap year timing. “The 2017 cap year will start on October 1, 2016 and end on September 30, 2017,” according to the rule schedule for publication in the Aug. 5 Federal Register. The change aligns the cap accounting year with the federal fiscal year, CMS notes in its release.
Watch out: The change “will have an impact on when hospices must submit their self-calculated Aggregate Cap starting with the 2017 Cap Report,” NAHC warns in its member newsletter. Hospices must “complete their aggregate cap determination not sooner than 3 months after the end of the cap year, and not later than 5 months after, and remit any overpayments,” CMS reminds providers in the rule. “Those hospices that fail to timely submit their aggregate cap determinations will have their payments suspended until the determination is completed and received by the Medicare Administrative Contractor.”
Resource: Check out Table 26 in the rule, which outlines how to count beneficiaries for the cap during the transition time frame.
No Exceptions To New CBSAs
Another reimbursement-related change is the full adoption of Office of Management and Budget Core Based Statistical Area delineations. One agency protested its CBSA make-up, but CMS shot down the complaint. “We believe that the OMB’s CBSA designations reflect the most recent available geographic classifications and are a reasonable and appropriate method of defining geographic areas for the purposes of wage adjusting the hospice payment rates,” CMS says in the final rule. “We do not see any compelling reason to deviate from the OMB designations.”
This year’s rule contained relatively few reimbursement changes, compared to last year’s rule with sweeping hospice payment reform including the splitting of the Routine Home Care payment rate and addition of Service Intensity Add-on payments. This year’s rule was more focused on quality items (see related stories, this issue).
Note: The final rule is at https://s3.amazonaws.com/public-inspection.federalregister.gov/2016-18221.pdf.
Home Health & Hospice Week
- Pre-Claim Review:
This Is Not A Test
PCR demo launches in initial state. As the Aug. 1 launch date for the pre-claim [...] - Hospice:
Hospice 2017 Pay Increase Improves Slightly To 2.1%
Pay raise will add an estimated $350 million to hospice payments next year. If you [...] - Quality:
It's Official: 2 New Quality Measures Adopted For Hospice
Start collecting new HIS item data April 1. Get ready to answer for your visit [...] - Hospice:
Get To Know Your 9 Hospice Quality Measures
One new measure is a star rating proxy. And then there were nine. The Centers [...] - Quality:
Final Rule Includes More Hospice Compare Details
HIS and CAHPS data both will make the Hospice Compare cut. The biggest change in [...] - Hospice Item Set:
Hospice Assessment Tool Coming, Despite Concerns
Can hospices shoulder the extra burden? Hospices are not convinced that a patient assessment tool [...] - Reimbursement:
Timely Reporting Threshold Jumps To 80% Jan. 1
Access new HIS report to keep tabs on your compliance. It’s time to tighten up [...] - Human Resources:
Boost Retention With Employee Appreciation Day
A low-cost activity can yield big benefits. Appreciation is one of the most powerful motivation [...] - Industry Note:
F2F Fuels Agency's Alleged $7.5 Million Overpayment
OIG auditors seize on physician narrative. Are you prepared for the HHS Office of Inspector [...] - Industry Note:
MAC Investigates Reported Claims Payment Errors
Meanwhile, other claims glitches still go unexplained. HHH Medicare Administrative Contractor CGS is also experiencing [...] - Industry Note:
DOL Increases FLSA Penalty Amounts Significantly
Watch out for increased penalty amounts from the Department of Labor taking effect this month. [...]

