Prepare for 2021 E/M Changes That Will Affect Your Surgery Practice

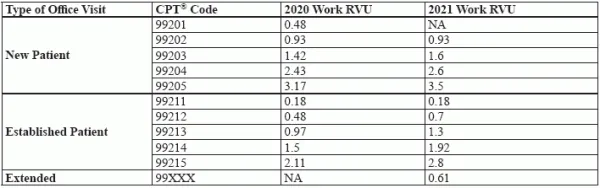
Grasp now and then with case example. How your surgeons report outpatient E/M services is in the midst of an overhaul driven by CMS rules and CPT® changes. Let our experts give you the big picture so you understand what you should be doing now, what you’ll need to do in 2021, and how the changes might impact your practice’s bottom line. You Should Be Doing This Now Although the biggest E/M reporting challenges won’t take effect until 2021, you should already be implementing certain changes regarding E/M documentation. For documenting history, including chief complaint (CC); past, social, family history (PFSH); review of systems (ROS); and history of present illness (HPI), the following changes outline who can document these components in the medical record for new and established office/outpatient visits: Additionally, if your surgeon chooses a home visit instead of an office visit, you no longer need to document medical necessity. Coder tip: If you haven’t already done so, you might want to contact your Medicare Administrative Contractors (MACs) to determine what, exactly, they will be looking for with these new documentation guidelines, suggests Suzan Hauptman, MPM, CPC, CEMC, CEDC, director of compliance audit at Cancer Treatment Centers of America. Prepare for 2021 Changes You won’t implement the biggest changes to E/M coding until next year, but you should learn the facts now and get ready. Here’s what you need to know for billing new and established patient office/outpatient services next year: Exception: “CMS … is not making any changes to the E/M office visits captured in the 10-day and 90-day global codes,” states Miranda Franco, senior policy advisor with Holland & Knight LLP in Washington D.C., in the Holland & Knight healthcare blog. Preview Pay Changes With the revised 2021 CPT® codes, CMS will also adopt the AMA Specialty Society Relative Value Scale Update Committee (RUC)-recommended relative value units (RVUs) for the codes. These values represent higher work RVUs for most office/outpatient E/M codes, as you can see in the following table: Bonus: You can see from the table that your surgeons’ pay may increase for office/outpatient E/M visits in 2021. Other shoe: To achieve budget neutrality, CMS will have to decrease pay for some other services to balance increased pay for E/M. Depending on those changes, which CMS has not announced, and the procedure profile for your surgeons, this E/M overhaul could be a net pay loss or a net pay gain for your practice. Although CMS provides Table 120 in the Medicare Physician Fee Schedule 2020 final rule to show specialties that might see the most positive and negative pay impact, the agency qualifies the information as very tentative: “We believe these estimates provide insight into the magnitude of potential changes for certain physician specialties, but note that Table 120 does not take into account other changes to payment rates finalized for CY 2020 and should be considered for illustrative purposes only,” the final rule advises. The table ranges from +16 percent impact for endocrinology to -10 percent impact for ophthalmology. General surgery isn’t represented in the table, indicating CMS expects a more moderate impact for that specialty. Check Out This Example Let’s look at the impact of the proposed change to CPT® code 99213, which is the most common established patient office code used across surgery practices. Current definition: Office or other outpatient visit for the evaluation and management of an established patient, which requires at least 2 of these 3 key components: o An expanded problem focused history; Counseling and coordination of care with other physicians, other qualified health care professionals, or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. 2021 definition: Office or other outpatient visit for the evaluation and management of an established patient, which requires a medically appropriate history and/or examination and low level of medical decision making. When using time for code selection, 20-29 minutes of total time is spent on the date of the encounter. Example: Surgeon’s note states, “Patient with long-term established tracheostomy presents with complaint of redness and pus from the tracheostomy. Reviewed history of [date of last visit] and remarkable changes include redness and yellowish secretions from the trach site. Normal heart and lung sounds, pulse 78, temperature 98.9, blood pressure 146/82, abdomen soft, no swelling in extremities, noted general pallor. Ordered culture of trach secretions, cleaned and replaced tracheostomy tube.” Now: Under current rules, the MDM in this case is low complexity (limited amount or complexity of data, low risk of complications and/or morbidity/ mortality). Without documentation of an extended problem focused history, you currently need all the details in the note documenting an expanded problem focused exam to establish the second key component that warrants coding 99213. 2021: In 2021, you’ll need to document a medically necessary and clinically appropriate history and exam, but these elements will not guide your code selection. Instead, you’ll choose your E/M code level based on either time spent or MDM. To earn 99213 without using time, you’d need to document two of the following three components: The note in this example still earns 99213 in 2021 by documenting the first and third of these elements, but you can see that under the new guidelines, including more detail regarding amount and complexity of data in this case would be beneficial.
o An expanded problem focused examination;
o Medical decision making of low complexity
Usually, the presenting problem(s) are of low to moderate severity. Typically, 15 minutes are spent face-to-face with the patient and/or family




