General Surgery Coding Alert
Use This FAQ to Strengthen Inpatient Coding Skills
Time is different in the hospital.
Just because you’re focused on CPT® 2021’s big changes to office or other outpatient E/M, you can’t afford to lose pay by letting your inpatient E/M coding skills get rusty.
Inpatient E/M codes 99221-99223/99231- 99233 (Initial/Subsequent hospital care, per day, for the evaluation and management of a patient …) and 99234-99236 (Observation or inpatient hospital care, for the evaluation and management of a patient …) don’t change in 2021, but they always create plenty of problems for coders. That’s why we assembled all of your most frequently asked questions about the services and asked some experienced inpatient coders to answer them.
Question: When Should I Use 99221-99223 versus 99234-99236 for Inpatient Care?
Answer: “The basic difference between the code [families] is that 99234-99236 represent the services of an initial hospital service and a discharge service performed on the same calendar date,” says JoAnne M. Wolf, RHIT, CPC, CEMC, coding manager at Children’s Health Network in Minneapolis. This means your documentation must reflect the exact times for admission and discharge.
“To bill 99234-99236, you must have a statement that shows the stay for observation care or inpatient hospital care was greater than eight hours but less than 24 hours,” advises Jessica Miller, CPC, CPC-P, CGIC, manager of professional coding for Ciox Health in Alpharetta, Georgia. “If the admission is greater than 24 hours, then you would use 99221-99223 for the initial day of hospital care,” Miller adds.

Question: When Can I Bill for Hospital Care?
Answer: Knowing which provider can, and cannot, bill these codes is often a confusing subject for inpatient care. But one easy way to break it down is to remember that “for the inpatient initial visits, only one physician can be the admitting physician and only the admitting physician can use codes 99221-99223,” Miller says.
All other providers should bill the inpatient E/M codes that describe their participation in the patient’s care. That includes subsequent hospital care codes 99231-99233 or inpatient consultation codes 99251-99255 (Inpatient consultation for a new or established patient …).
Example: “If Provider A sees the patient in the morning and Provider B, who is covering for A, sees the same patient in the evening, the notes for both services are combined and only one subsequent hospital visit is coded. However, if two physicians see the patient and they are in different specialties and are seeing the patient for different reasons (i.e., different diagnosis), then both may bill a subsequent hospital visit based on that physician’s note and the medical necessity of the service,” Miller adds.
Question: What Documentation Drives Hospital-Care Code Selection?
Answer: For hospital care codes, you must have documentation of the three key components of history, examination, and medical decision making (MDM), and you must match the documentation to the appropriate level for the code you select.
Coding alert: Remember that unlike the office and outpatient E/M codes, using the three key components for code selection will not change in 2021 — you will not be able to choose the level of hospital care based on MDM alone.
In addition to the three key elements, documentation in the medical record should include a statement of the total time for the care, and personal documentation by the billing provider indicating presence and face-to-face services, plus written admission and discharge notes, according to Miller.
Additionally, “because 99234-99236 represent both observation and hospital services, the documentation should support both services. That’s why I refer to these codes as ‘the combo codes,’” Wolf adds.
Question: What Does, and What Does not, Count for Time?
Answer: Like the revised 2021 office and outpatient E/M guidelines, you also have the choice to document hospital care based on time. However, this can lead to some problems when reporting the codes. “Time is often underreported for inpatient E/M services. Providers don’t always remember to document time that is spent on the unit/floor that is outside the face-to-face time with the patient and family,” notes Wolf.
Key: Per CPT® guidelines, “unit/floor time … includes the time present on the patient’s hospital unit and at the bedside rendering services for that patient. This includes the time to establish and/or review the patient’s chart, examine the patient, write notes, and communicate with other professionals and the patient’s family.”
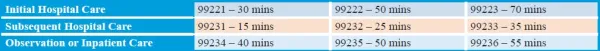
Another important thing to remember is that the typical times for the hospital codes are all different, as the following chart shows:
Related Articles
General Surgery Coding Alert
- E/M 2021:
Use This FAQ to Strengthen Inpatient Coding Skills
Time is different in the hospital. Just because you’re focused on CPT® 2021’s big changes [...] - CPT® 2021:
Update Your Breast Reconstruction/Repair Coding Know-How
Drill down to significant code revisions. With 15 revised codes and two code deletions, pl.us [...] - HIPAA:
Protect Patient Information Beyond the Chart
Understand compliance relief during PHE. Even though you can share patient protected health information (PHI) [...] - You Be the Coder:
Beware Swan-Ganz Bundles
Question: Our surgeon performed a Swan-Ganz procedure, placed a central line through the same incision, [...] - Reader Questions:
Clarify ‘Correlates’ and ‘Consistent’ Dx Terminology
Question: When I’m assigning a diagnosis code, I’m always confused when the surgeon documents a [...] - Reader Questions:
Select Most Specific EGD Procedure Code
Question: A patient was referred to our surgeon for suspected esophageal cancer or abnormality. The [...] - Reader Questions:
Illegible Signature?
Question: What can we do our surgeon’s signature is illegible? Oregon Subscriber Answer: You can [...]




