General Surgery Coding Alert
Delve Deeper For Hernia Repair Coding Update
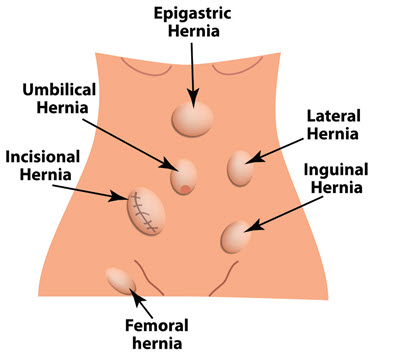
Know size measurement rules. After a few months of coding hernia repairs using the CPT® 2023 revisions, you may have some remaining questions about how to implement all the changes. Read on to get details about the anterior abdominal hernia repair codes, and to learn essential documentation tips for accurate reporting. Background: We briefly outlined the hernia coding overhaul in General Surgery Coding Alert Vol. 24 No. 10, “Jumpstart Your 2023 Readiness With This Coding Preview.” Recall that CPT® deleted open hernia repair codes 49560-49566 (Repair … incisional or ventral hernia …), 49570-49572 (Repair epigastric hernia …), 49580-49587 (Repair umbilical hernia …), 49590 (Repair spigelian hernia); as we; as laparoscopic hernia repair codes 49652-49653 (Laparoscopy, surgical, repair, ventral, umbilical, spigelian or epigastric hernia …) and 49654-49657 (Laparoscopy, surgical, repair, … incisional hernia …). To replace these codes, CPT® created a more unified category that encompasses open or laparoscopic epigastric, incisional, ventral, umbilical, and spigelian hernia repair. Review the New Codes For any hernia repair in the new “anterior abdominal hernia” category, you’ll report one of the following 12 new codes, which CPT® 2023 distinguishes based on initial or recurrent, reducible or incarcerated/strangulated, and repair size: Key: The codes break down into two groups based on whether the service is an initial hernia repair (49591-49596) or the repair of a recurrent hernia (49613-49618). Base Coding on Total Defect Size Under the new codes, if the surgeon repairs multiple anterior abdominal hernias in a single surgical session, you should select just one repair code. Do not individually report each hernia repair using a separate code. “These codes [49591-49596 and 49613-49618] are reported only once, based on the total defect size, for however many abdominal hernias the patient has that are getting repaired in that surgical session,” said Kelly Shew, RHIA, CPC, CPCO, CDEO, CPB, CPMA, CPPM, CRC, documentation and coding education, Olympia Medical in Livonia, Michigan, in the March 15 AAPC Ask & Learn Webinar titled “2023 Changes for Hernia Coding.” Key: Instead of a single code for each hernia, you should choose the proper code based on the total measurement of all the hernias repaired. The surgeon should take the measurement before opening the patient, “because the fascia can retract during the repair and the measurement would be falsely elevated,” Shew said. Single: For a single hernia, you’d select the code based on the documented measurement of the pre-surgical hernia’s longest length. Measure multiple: For multiple non-contiguous defects separated by greater than or equal to 10 cm of intact tissue, calculate the defect size for coding purposes as the sum of each individual hernia. However, if the separate defects are within 10 cm of each other, you should measure “from the furthest point to the furthest point [of the multiple defects] and use that total length,” said Elizabeth Herbert, RHIA, CPC, CPMA, CRC, CCC, CPC-I, Epic Application Analyst at Baptist Health System in Scottsburg, Indiana during the AAPC Ask & Learn Webinar. Mixed multiples: Because the codes separate based on whether the hernia is reducible or incarcerated/strangulated, what should you do if you’re adding the length of multiple hernias when one is reducible and one is strangulated? “If the surgeon repairs reducible and incarcerated/strangulated hernias at the same operative session, add the lengths and report the service using the appropriate incarcerated/strangulated code,” says Terri Brame Joy, MBA, CPC, COC, CGSC, CPC-I, product manager, MRO, in Philadelphia. Example: The surgeon performs three incisional hernia repairs in a single session. The cranial (toward the head) defect involves a 2 cm reducible hernia. Moving 3 cm in the caudal (toward the feet) direction, the surgeon repairs one, 4 cm incarcerated hernia, and 2 cm caudally, repairs another 3 cm reducible hernia. The total distance between the two farthest points of the three defects is 14 cm. That means you should report the service as 49596. Other hernias: Because of nature of the incision itself, you can separately report other types of hernia repair, such as for femoral, lumbar, inguinal, and parastomal hernias if done in the same surgical session, Shew clarified. Poor Documentation Can Cost You Money Your surgeon’s documentation must show total defect size for you to accurately report an anterior abdominal hernia repair code. And because the surgeon must determine the measurement before opening the patient, documentation is more important than ever. If the documentation is vague, your only choice is to query the surgeon or report a lesser code. For instance, if the op report states that the reducible hernia is approximately 3 cm, which is right on the cusp between codes, you will likely need to play it safe and report the code for a hernia that’s less than 3 cm, which is 49591 for an initial repair rather than 49593 if the surgeon had accurately reported 3.5 cm. The payment for those two codes is $345.65 and $579.13 respectively (Medicare Physician Fee Schedule National payment amount, conversion factor 33.8872). That means missing accurate documentation would cost the surgeon $233.48. Too late: Even if you were to query the provider, there’s no way they can measure the pre-surgery hernia size retroactively. The same rings true if the provider did not report a measurement at all. You’ll have to report the lowest code possible for the type of hernia, whether initial or recurrent. Do this: The revised codes offer a good opportunity to initiate an educational conversation with your surgeons. Providers certainly want to get paid fairly, and that’s only possible with exact measurements.
Related Articles
General Surgery Coding Alert
- CPT® 2023:
Delve Deeper For Hernia Repair Coding Update
Know size measurement rules. After a few months of coding hernia repairs using the CPT® [...] - Recognize Impact of 0-Day Global Period
As you just read in “Delve Deeper For Hernia Repair Coding Update,” CPT® 2023 deleted [...] - Practice Management:
Refresh Your HIPAA Compliance Know-How
Waivers end with PHE. With the end of the COVID-19 public health emergency (PHE) this [...] - You Be the Coder:
Distinguish Lesion ‘Excision’ and ‘Destruction’ Codes
Question: The op report identifies a 1.5 cm basal cell carcinoma diagnosed by prior biopsy that [...] - Reader Questions:
Capture Mesh Removal
Question: Do the new anterior abdominal hernia repair codes include removal of mesh, if performed? Florida [...] - Reader Questions:
See The ESD EMR Difference
Question: During a colonoscopy, our surgeon documented removing a large colon polyp using endoscopic submucosal dissection [...] - E/M:
Follow This Expert Advice for Inpatient/Observation Codes
See when office care leads to ‘subsequent’ hospital care. With the overhaul of hospital inpatient/observation [...]