Capture Cannula Services for ECMO Patients
Your surgeon may be part of the life support team.
If you thought you could ignore CPT® 2015’s overhaul of extracorporeal membrane oxygenation (ECMO) codes because your surgeon doesn’t perform that service, you could be missing an opportunity.
That’s because the new CPT® ECMO/extracorporeal life support (ECLS) section offers specific codes for individual parts of the treatment that different physicians might complete. For instance, your general surgeon might perform the percutaneous cannula insertion and removal, even if she isn’t involved throughout the ECMO/ECLS procedure.
We’ll walk you through the new codes to make sure you capture any work that your general surgeon performs as part of the ECMO/ECLS healthcare provider team.
Understand the Treatment
The typical ECMO/ECLS patient used to be a premature newborn, but now ECMO/ECLS providers also often treat adults with severe flu, pneumonia, or respiratory distress syndrome, according to Peter K. Smith, MD, of the Society of Thoracic Surgery in his CPT® and RBRVS 2015 Annual Symposium presentation.
Old way: For ECMO/ECLS, you used to use 33960 (Prolonged extracorporeal circulation for cardiopulmonary insufficiency; initial day) and 33961 (… each subsequent day), but those codes are gone this year.
In place of 33960-33961, CPT® 2015 introduced more than two dozen new codes in the range 33947-33989 to describe ECMO/ECLS.
Depending on patient needs, the physician may choose a veno-arterial or veno-venous treatment. In veno-arterial ECMO/ECLS, the physician places one cannula, which is a thin tube, in a large vein and places one cannula in a large artery. This method can support both the heart and lungs.
For lung support only, the physician may choose veno-venous ECMO/ECLS. This method may involve one or two cannulae in the venous system.
The ECMO/ECLS treatment begins with “initiation,” which involves deciding which device components are correct for the patient, as well as the blood flow, gas exchange, and those sorts of necessary parameters. The physician performing this service chooses between these codes:
Daily management: For daily ECMO/ECLS management, the physician oversees the patient’s care to manage blood flow and gas exchange. He checks for clotting and bleeding issues, ensures the cannula or cannulae are in proper position, and ensures the machines are functioning properly. The codes again differ based on veno-venous (33948) and veno-arterial (33949).
Note that daily overall patient management is a distinct service that the performing provider may report using an E/M code.
Select Cannula Codes Based on Approach and Age
CPT® now has specific codes for cannula insertion, repositioning, and removal associated with ECMO/ECLS treatment. These are procedures that your general surgeon might perform even if he isn’t treating the patient’s underlying condition or monitoring the ECMO therapy. The cannula procedure codes vary based on patient age and surgical method.
For patients from birth to five years, choose from the following codes depending on whether the approach is percutaneous, open, or by sternotomy/thoracotomy:
For patients six years and older, choose from these codes:
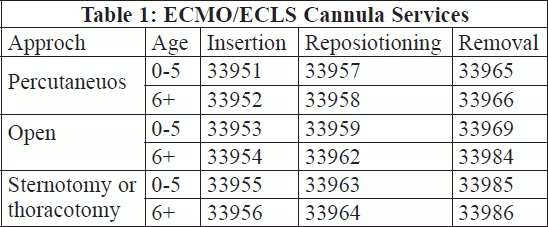
Report repositioning/removal: Like the insertion codes, the distinction between each of the cannula repositioning and removal codes depends on age and approach, as you can see in Table 1:
Caution: If your surgeon performs a cannula insertion, repositioning, or removal associated with ECMO/ECLS, you must use the codes from this section. You should not report other cannula or catheter codes such as 36800-36815 (Insertion of cannula for hemodialysis, other purpose [separate procedure]; …).
Look for Other Open Surgical Codes
If you code for open procedures, you should also be aware of +33987 (Arterial exposure with creation of graft conduit [e.g., chimney graft] to facilitate arterial perfusion for ECMO/ECLS [List separately in addition to code for primary procedure]), which you may use with open insertion codes 33953-33954 and sternotomy/thoracotomy insertion codes 33955-33956.
If your surgeon inserts or removes a vent that helps keep the heart chamber from distending, you should be familiar with codes 33988 (Insertion of left heart vent by thoracic incision [e.g., sternotomy, thoracotomy] for ECMO/ECLS) and 33989 (Removal of left heart vent by thoracic incision [e.g., sternotomy, thoracotomy] for ECMO/ECLS).
Safeguard Your Claims’ Accuracy With These Rules
To apply the cannula service codes in real world situations, you need to understand a few rules.
Removal/insertion: To report cannula replacement (removal and then insertion in the same vessel), use the insertion code. But if the physician removes a cannula from one vessel and puts a new cannula in a different vessel, report both removal and insertion codes.
Repositioning rules: You can’t always separately bill a cannula repositioning service. Initiation includes daily management and repositioning. This rule applies even when different physicians provide the services. For instance, if your surgeon performs repositioning on the same date that another provider bills initiation for the same patient, it would be incorrect for you to report repositioning, according to CPT® guidelines.
Also, you may not report cannula repositioning at the same session as insertion. Nor should you separately report fluoroscopic guidance, because the codes for cannula repositioning include related fluoro.
Insertion plus: A single physician may report insertion, initiation, and an E/M code for overall management on the same date.