Gastroenterology Coding Alert
You Be the Coder:
E/M Service Before a Procedure? Choose the Modifier Wisely
Published on Tue Feb 16, 2016

You’ve reached your limit of free articles. Already a subscriber? Log in.
Not a subscriber? Subscribe today to continue reading this article. Plus, you’ll get:
- Simple explanations of current healthcare regulations and payer programs
- Real-world reporting scenarios solved by our expert coders
- Industry news, such as MAC and RAC activities, the OIG Work Plan, and CERT reports
- Instant access to every article ever published in Revenue Cycle Insider
- 6 annual AAPC-approved CEUs
- The latest updates for CPT®, ICD-10-CM, HCPCS Level II, NCCI edits, modifiers, compliance, technology, practice management, and more
Related Articles
Other Articles in this issue of
Gastroenterology Coding Alert
- Procedural Coding:
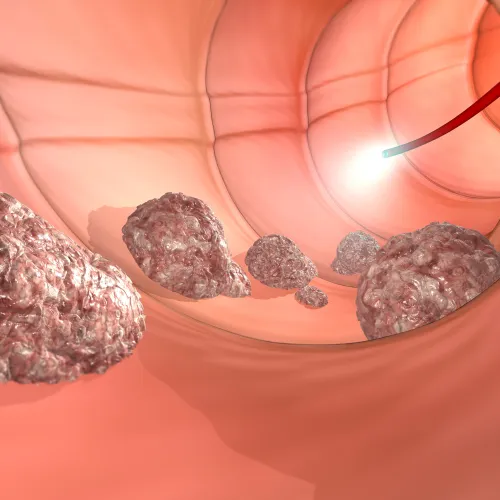
Check These 4 Pre-Requisites for a Perfect Proctosigmoidoscopy Claim
Follow Endoscopic family rules for any therapeutic services during the procedure. Your gastroenterologist might sometimes [...] - Medicare Fees:
Prepare for Physician Pay Cuts in 2016 MPFS Recommendations
Endoscopy sees maximum fee cuts. If you are rejoicing over the news that the Sustainable [...] - E/M Errors:
Take Corrective Action Fast to Reduce Possibly Inflated E/M Claims that CERT has Flagged
Even NPP claims are equal culprits. Audit studies have always found evaluation and management coding [...] - You Be the Coder:
E/M Service Before a Procedure? Choose the Modifier Wisely
Question: We have many cases where the physician decides to perform a procedure later the same [...] - Readers Question:
Include Tube Removals as Part of E/M Services
Question: Our gastroenterologist performed EGD on a patient on one day and colonoscopy along with PEG [...] - Reader Question:
Don't Drop 'Z' Code for Screening Colonoscopy
Question: Our surgeon performed a screening colonoscopy for a Medicare patient, but found and treated a [...] - Reader Question:
ERCP + Injection Therapy for Papillotomy Most Likely a No No
Question: How should I report an ERCP (endoscopic retrograde cholangiopancreatography) with stent placement and injection therapy [...]
View All