Stagger the Diagnosis Codes Carefully When Reporting Screening + Treatment
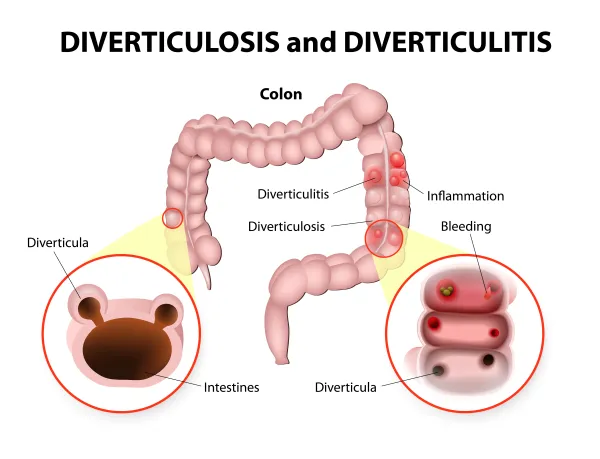
Question: While performing a screening colonoscopy, our GI found polyps and treated them. His notes indicated a diagnosis of benign colon polyps. The notes also mentioned that the patient had diverticulosis. Should I put the Z code for screening for malignant neoplasm as a third diagnosis? In the past, Medicare has kicked the claim out and won’t pay if I put the Z code on, but that seems to be a proper code. What should I do?
Nebraska Subscriber
Answer: If the physician’s documentation states that the patient presented for screening colonoscopy, you need to have the Z code (such as Z12.11, Encounter for screening for malignant neoplasm of colon) as the first diagnosis even if the physician found and treated other problems. Medicare has been pretty clear that if the patient presents for screening you have to bill the screening with the Z code, even if the physician finds a problem and treats it.
When the physician finds and treats a problem, you can no longer report the G codes (G0104-G0105, Colorectal cancer screening) for the screening colonoscopy. You do still need to list the Z code as the patient’s primary diagnosis in box 21 of the CMS-1500 claim form.
Tip: Just because the Z code is your primary diagnosis, however, does not mean that you have to link that diagnosis in the first position on your claim. Medicare expects coders to follow the coding guidelines for diagnosis codes, but the line-by-line links do not have to be in that order.
To avoid denials you should list the polyp diagnosis code (D12.-, Benign neoplasm of colon, rectum, anus and anal canal) in the first position to describe the medical necessity for the service.
Alternative: Of course, the definition of a screening colonoscopy is a colonoscopy for a patient that presents without symptoms. If this was really a diagnostic colonoscopy because the patient was having pain or bleeding due to his diverticulosis, that changes the coding and reimbursement entirely.
In that case, you should code a colonoscopy with polypectomy (such as 45384, Colonoscopy, flexible; with removal of tumor[s], polyp[s], or other lesion[s] by hot biopsy forceps) and attach the diverticulosis (K57.30, Diverticulosis of large intestine without perforation or abscess without bleeding) and colon polyp (D12.-) diagnoses.