Gastroenterology Coding Alert
Learn What’s Needed for Showing Necessity
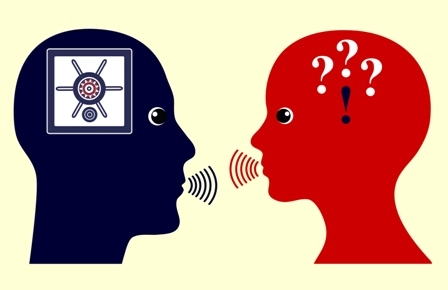
Question: My provider said that as long as we include a diagnosis code for a condition, that’s enough to justify medical necessity for the service. I’m not sure that’s true, but I don’t know how to talk to my provider about it. Could you please advise?
California Subscriber
Answer: You can’t justify medical necessity by simply assigning a particular diagnosis code to a claim. Seeing a specific ICD-10-CM code listed on a local coverage determination (LCD) or payer policy and assuming that as long as the patient’s diagnosis code matches that, then approval is a sure thing, may be common. That’s not accurate, however.

Let’s first review medical necessity and what it really means. According to the Centers for Medicare & Medicaid Services (CMS), “Medical necessity of a service is the overarching criterion for payment in addition to the individual requirements of a CPT® code. It would not be medically necessary or appropriate to bill a higher level of evaluation and management service when a lower level of service is warranted. The volume of documentation should not be the primary influence upon which a specific level of service is billed. Documentation should support the level of service reported” (source: www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c12.pdf).
In other words, you need to report the correct diagnosis code(s) to support any services provided or tests performed, but explanations within the documentation that support quality of service, time spent, or specifics related to medical decision making must be included to justify the level of service.
Remember that the documentation needs to be informative and relevant, not just plentiful.
Ongoing education and open communication continue to be essential as we move forward and as everyone grows accustomed to the evolving language within the evaluation and management (E/M) guidelines. Most providers aren’t familiar with the fine details outlined in the guidelines, but a little discussion can go a long way. For specific tips on how to talk with your provider in productive and respectful ways, check out this AAPC blog post: www.aapc.com/blog/42129-42129/.
Related Articles
Gastroenterology Coding Alert
- News You Can Use:
Review the Revamped Office/Outpatient Consultation Codes, Part 2
Get the scoop on consult reimbursement. Last month, Gastroenterology Coding Alert outlined the updated office/outpatient [...] - CPT® Coding:
Still Puzzled By These 2022 Endoscopic Procedure Codes? Here’s Help
Check out expert tips on how to scour the documentation. Ten months after their integration [...] - E/M Coding:
Follow This Advice to Correctly Code for Time
Compare these auditor red flags with your practice’s processes. Determining the level of an evaluation [...] - You Be the Coder:
Understand What to Do With Ruled-out Diagnoses
Question: The gastroenterologist suspected Barrett’s esophagus, which prompted an upper GI. Ultimately, the physician found [...] - Reader Questions:
Know When to Report Signs and Symptoms
Question: Our gastroenterologist referred a patient to a radiologist for an abdominal CT scan because of [...] - Reader Questions:
Learn What’s Needed for Showing Necessity
Question: My provider said that as long as we include a diagnosis code for a [...] - Reader Questions:
Know Who Needs to Provide Documentation
Question: My provider looked to another provider for their opinion on one of our patient’s [...]