2018 Medicare Fee Schedule Proposes Major Updates to E/M Documentation
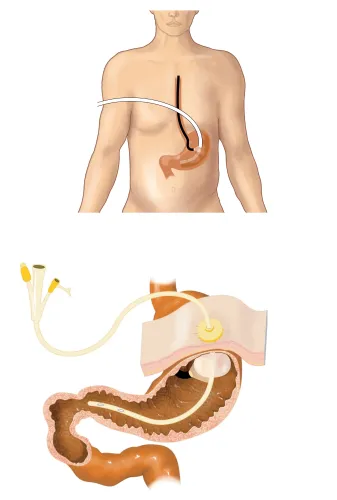
Plus: Check out these potential new esophagectomy codes. CMS has released its 2018 proposed Medicare Physician Fee Schedule, which recommends updates to the Part B payment policy. The proposals could be significant for gastroenterology practices, since some of the biggest revisions involve completely overhauling how E/M codes are selected Potential E/M Documentation Changes The proposed rule indicates that CMS is looking at updating the E/M code requirements for the first time in decades. “We are specifically seeking comment on how we might focus on initial changes to the guidelines for the history and physical exam because we believe documentation for these elements may be more significantly outdated, and that differences in medical decision-making (MDM) are likely the most important factors in distinctions between visits of different levels,” CMS says on page 377 of the proposal. CMS is not only suggesting that it might lean more heavily on MDM when selecting an E/M level, but even appears to be considering eliminating history and physical exam documentation requirements entirely. “We are also specifically seeking comment on whether it would be appropriate to remove our documentation requirements for the history and physical exam for all E/M visits at all levels,” the proposal says. “We believe medical decision-making and time are the more significant factors in distinguishing visit levels, and that the need for extended histories and exams is being replaced by population based screening and intervention, at least for some specialties.” Leaning Into MDM Could Benefit GI Practices CMS’ proposal may be shocking to many in the coding industry, but could have many positive impacts if finalized. The proposal that time would be more important in selecting an E/M code could be helpful in some cases, such as when gastroenterologists spend more time with a patient educating them on dietary factors, which comes to play during gastric surgery preparation, said gastroenterology coder Catherine du Toit, CPC, CPMA, CGIC of Clean Claims Coding Consultants. In addition, the change could prompt gastroenterologists to more carefully assess the MDM in their medical records when selecting a code. “Auditing GI services for the past 11 years, I do not think that gastroenterologists rely too much on MDM — maybe they should,” du Toit said. “History, especially history of present illness (HPI) and past medical, family, and social history (PFMSH), are extremely important to determine the status for average risk screening/high risk screening services. Erroneous claim submissions can lead to a big loss in revenue.” Submit Comments to Have Your Say Although some practices are cheering the lower documentation burden that this could create, others are questioning why CMS would loosen the requirements for an area of coding that already has challenges. “Removing the history and physical (H&P) component from coding guidelines is like having a tree with no ‘roots,’” suggests Vinod Gidwani, president of full-service revenue cycle firm Currence, based in Skokie, Illinois. “The H&P determines the level of medical decision-making as well as the time component. Removing the H&P is like determining the MDM and time components in a vacuum,” Gidwani says. Medical societies and the CPT® Panel have been very cautious ever since the 1997 E/M documentation guidelines were published by CMS because the simplification of code structure or of documentation requirements raises concerns whether there would be an accompanying downward revaluation of E/M code reimbursement, says Glenn Littenberg MD, former CPT® Panel member. “Philosophically I’m very much in favor of changes that would simplify physician documentation work if isn’t clinically relevant and only exists to support the code level chosen,” Littenberg says. “I certainly don’t see that the true work of E/M encounters has changed, though there is probably more time spent before and after the face-to-face service. How CMS might wish time is documented and whether CPT® and the RUC might need to revisit code descriptors, typical times, and therefore work RVUs, should concern all of us who care about a fair fee schedule.” No matter where you stand on this issue, CMS wants to hear from you. “We are seeking comment on whether clinicians and other stakeholders believe removing the documentation requirements for the history and physical exam would be a good approach,” the agency says in the proposal. If your practice has an opinion on this matter, now is a good time to submit your comments, which are due by Sept. 11, 2017. You can either submit online at www.regulations.gov (referencing CMS-1676-P), or by mail or in person. New Esophagectomy Codes Revealed The proposal also lists suggested relative value units (RVUs) for three new esophagectomy codes that appear to be slated for a Jan. 1, 2018 debut. Although the fee schedule doesn’t reveal the exact CPT® codes assigned to the new codes, the following details are shared in the proposal: In the past, coders had to report an unlisted code for laparoscopic esophagectomies, so the above new codes will definitely come in handy for GI coders if finalized. Resource: To read the proposed fee schedule, visit https://s3.amazonaws.com/public-inspection.federalregister.gov/2017-14639.pdf.