Gastroenterology Coding Alert
Make the Most of the Four "Pick Your Own Pace Options" From CMS
Start work now on colonoscopy and GERD, says AGA.
Washing away all the speculations about a MACRA delay, CMS acting administrator Andy Slavitt has made it clear that go-live date of the new value-based reimbursement program will be January 2017. CMS estimates that about 12,600 GIs will be subject to MIPS and up to 38.3 percent of the providers may be subject to penalties. You will need to prepare now for success in the new quality driven payment model. Plan now to avoid cuts.
Good news: To ensure that all eligible clinicians have the opportunity to succeed under MACRA’s Quality Payment Program, CMS plans to allow physicians to pick their pace of participation for the first performance period that begins January 1, 2017. “This flexibility is welcomed by most gastroenterology practices who do not have current opportunities to participate in Alternative Payment Models and will have trouble meeting the MIPS reporting methods that are more applicable to primary care practices,” says Michael Weinstein, MD, former representative of the AMA’s CPT® Advisory Panel.
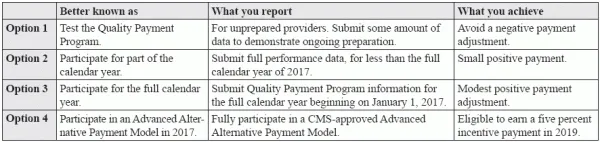
Based on your level of preparedness, you will have the freedom to choose between four flexible reporting tracks in the first performance year, allowing you to avoid a negative payment adjustment in 2019.
These options are being welcomed by the providers, “because it gives practices options for choosing MIPs or APMs,” says Catherine Brink, BS, CMM, CPC, CMSCS, CPOM, president, Healthcare Resource Management, Inc. Spring Lake, NJ. The “decision should be based on the demographicsof the practice, the percentage of patients who are covered by Medicare, and whether the practice consists of a non-par provider.”
Pick One of the Options to Suit Your Pace
These four reporting tracks, which expand the options for participating in the MIPS program, offer eligible clinicians different levels of data reporting.
Explore the Opinions Galore
Many providers feel that new MACRA flexibilities for the first performance year of the program may help them ease into new value-based reimbursement programs. However, some remain skeptical.
The welcome approach: “By adopting this thoughtful and flexible approach, the Administration is encouraging a successful transition to the new law by offering physicians options for participating in MACRA,” said Andrew W. Gurman, MD, AMA President, in an AMA news release on Sept. 8.
The skeptical approach: However, the American Medical Group Association (AMGA) feels otherwise. For the providers that have already prepared for the program. “… new reporting options will have the unintended result of penalizing the very provider groups that have made the largest investments to meet MACRA’s goals of better quality, improved clinical practice activities, better use of electronic medical records, and lower resource use,” said Donald W. Fischer, PhD, CAE, AMGA President and CEO, in an AMGA news release on Sept. 12.
Start Work on Colonoscopy and GERD Reporting
Successful reimbursement for Colonoscopy screening and surveillance, gastroesophageal reflux disease (GERD) or Barrett’s Esophagus (K22.70-), viral hepatitis (category B15.- to B19.-) and obesity (E66.-), are on the agenda of the American Gastroenterological Association (AGA), and AGA has proposed payment models for inclusion in the MACRA quality payment system.
Take action: “Gastroenterology practices must continue to lobby to have MACRA rules that provide them an opportunity to fully participate and provide meaningful measures data that improves patient care,” says Weinstein. “There is a lot of work needed to develop MIPS measures and APMs. Gastroenterology practices must support the work of their societies and advocacy associations and provide feedback about the proposed methods as information is released.”
Editor’s note: Look out for the ways to start preparing for reporting colonoscopy and GERD in alignment with MACRA directives, in the next issue.
Related Articles
Gastroenterology Coding Alert
- CPT® 2017 Update:
Get the Pulse of CPT® 2017 Final Updates for Gastroenterology
Be ready for removal of conscious sedation from 43235, 43260, and many more changes… The [...] - ICD-10 Update:
Master the New ICD-10 Codes for Intestinal Infarcts, Hepatic Failure and Pancreatitis
New options for pancreatitis let you code based on presence of necrosis October is here [...] - MACRA Update:
Make the Most of the Four "Pick Your Own Pace Options" From CMS
Start work now on colonoscopy and GERD, says AGA. Washing away all the speculations about [...] - You Be the Coder:
Know How to Code For Incomplete Colonoscopy
Question: A provider performs diagnostic colonoscopy. During the procedure, he is able to progress the colonoscope [...] - Reader Question:
Explore Coding Options in Endoscopic Ultrasound (EUS) Along With FNA
Question: The provider performs endoscopic ultrasound with optical endomicroscopy (OE) and fine needle aspiration of a [...] - Reader Question:
Tread Carefully With Sclerotherapy for Esophageal Varices
Question: The doctor performs sclerotherapy for esophageal varices. How do we report this? Utah Subscriber Answer: In [...] - Reader Question:
Hit the Right Code for EGDs with Dilation and Biopsy
Question: Our surgeon performed an EGD that required dilation for access. Upon examination of the duodenum, [...] - Reader Question:
Explore Your Coding Options for Gastroesophageal Reflux Test
Question: A fifty year old male patient, complaining of heart burn, is diagnosed as having gastro-esophageal [...] - Reader Question:
Pick the Right Code for Transoral Esophagoscopy with Specimen Collection
Question: The provider views the esophagus by means of rigid endoscope through the mouth. He also [...]




