Your Diagnoses Will Prop Up Your G Codes for High Risk Colonoscopies
A hemorrhoid’s location should lead you to the appropriate ICD-10.
Want to get your hemorrhoid report right and stress-free? You can start by knowing the difference between internal and external hemorrhoids, but you can learn more from this sample physician’s report:
PREPROCEDURE DIAGNOSIS: History of colon polyps and partial colon resection, right colon.
POSTPROCEDURE DIAGNOSES:
1. Normal operative site.
2. Mild diverticulosis of the sigmoid colon.
3. Internal hemorrhoids.
PROCEDURE: Total colonoscopy.
PROCEDURE IN DETAIL: The 60-year-old patient presents to the office to be evaluated for the preprocedure diagnosis. The patient also apparently had an x-ray done at the hospital and it showed a dark spot, and because of this, a colonoscopy was felt to be needed. She was prepped the night before and on the morning of the test with oral Fleet’s, brought to the second floor and sedated with a total of 50 mg of Demerol and 3.75 mg of Versed IV push. Digital rectal exam was done, unremarkable. At that point, the Pentax video colonoscope was inserted. The rectal vault appeared normal. The sigmoid showed diverticula throughout, mild to moderate in nature. The scope was then passed through the descending and transverse colon over to the hepatic flexure area and then the anastomosis site was visualized. The scope was passed a short distance up the ileum, which appeared normal. The scope was then withdrawn through the transverse, descending, sigmoid, and rectal vault area. The scope was then retroflexed, and anal verge visualized showed some internal hemorrhoids.
RECOMMENDATIONS: Repeat colonoscopy in three years.
Let Stage or Grade Guide You
You can easily identify external hemorrhoids because of its place of appearance. This type of hemorrhoid has a fleshy growth and occurs around the anus -- specifically, outside the anal verge, which is at the distal end of the anal canal. On the other hand, internal hemorrhoids occur inside the anal canal. The veins lining the walls of the rectum become enlarged (blood clot) and bulge out.
Another way to distinguish internal from external hemorrhoids is by looking at their location compared to the dentate line. The line is a mucocutaneous junction about a centimeter above the anal verge and can be seen separating the anus from the rectum. While internal hemorrhoids take place above the dentate line, external hemorrhoids take place below the line.
Ideal: While you may learn to differentiate one hemorrhoid type from the other through years of practice, you could dodge coding errors by asking your physicians to indicate “internal” or “external” in their notes.
You should specifically look for the type of hemorrhoid as choosing the right code is principally based on the type of hemorrhoid i.e. internal, external or unspecified. So, you will need to know if the hemorrhoid is of internal or external type to correctly report it. When details about the type of hemorrhoid are not available you will need to report the condition under unspecified category.
In ICD-10, both hemorrhoids and perianal venous thrombosis are placed under one classification (K64, Hemorrhoids and perianal venous thrombosis) and this list includes piles too. However, this list does not include hemorrhoids complicating pregnancy (O22.40, Hemorrhoids in pregnancy, unspecified trimester) and hemorrhoids complicating childbirth and the puerperium (O87.2, Hemorrhoids in the puerperium).
While reporting internal hemorrhoids, you need to know the stage or the grade of the hemorrhoid. If the grade is not specified, then you need to report the condition under a different code. The presence or absence of prolapse also helps you decide the code.
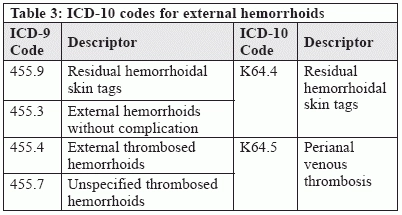
For external hemorrhoids, the presence of skin tags and thrombosis forms the important information on which you can report the condition.
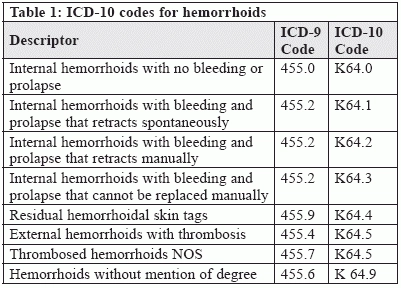
Look back at ICD-9: You have one-to-one codes for reporting hemorrhoids, both external and internal. Same applies to hemorrhoids that are thrombosed and the formation of residual skin tags (Table 1).
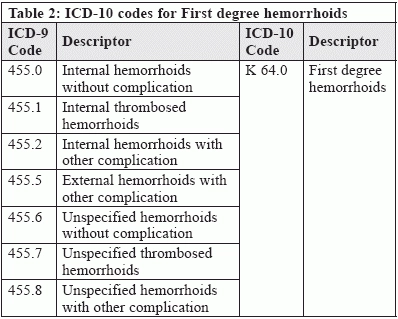
However, under ICD-10, depending on the grade, a single ICD-10 code is used to describe many different codes under ICD-9 (Table 2 shows example for first degree hemorrhoids). All these ICD-9 codes can also be used to represent K64.1 (Second degree hemorrhoids), K64.2 (Third degree hemorrhoids), and K64.3 (Fourth degree hemorrhoids) depending on the stage of the hemorrhoids. Your physicians may not realize that the new ICD-10 codes are chosen based on the hemorrhoid “grade” or “degree” and may not designate the grade in the report. If the usual report is missing the grade, then you should take the time to educate your physicians on the new codes and the importance of specifying the grade — especially if a therapeutic hemorrhoid procedure is performed.
In case of external hemorrhoids without complication and external hemorrhoids that form residual skin tags, it is reported under a single ICD-10 code (Table 3). In case of thromobosed external hemorrhoids, you report the condition using K64.5 (Perianal venous thrombosis).
Tread Through Hemorrhoid Excision Codes Cautiously
By adding the following text note, CPT® gives you the permission to use certain codes for excision of internal and/or external hemorrhoids: “For excision of internal and external hemorrhoids, see 46250-46262, 46320.” This means you can opt for 46255 (Hemorrhoidectomy, internal and external, single column/group) or 46260 (Hemorrhoidectomy, internal and external, 2 or more columns/groups) for excision of multiple internal hemorrhoids.
You may go for 46945 (Hemorrhoidectomy, internal, by ligation other than rubber band; single hemorrhoid column/group) or 46946 (Hemorrhoidectomy, internal, by ligation other than rubber band; 2 or more hemorrhoid columns/groups) for some internal hemorrhoid excisions.
How it’s done: Known as “transfixion suture excision,” the surgeon places a crisscross stitch and ties off the base of the hemorrhoid with the suture (ligation) to take control of the bleeding. Post this, the surgeon excises and removes the remaining hemorrhoid.
Alternatives: Sometimes a physician would inject solution to cause the hemorrhoid to harden and shrivel. In this case, you should report 46500 (Injection of sclerosing solution, hemorrhoids). For thermal destruction, you should bill 46930 (Destruction of internal hemorrhoid[s] by thermal energy [e.g., infrared coagulation, cautery, radiofrequency]). CPT® 46999 (Unlisted procedure, anus) would fit a destruction by cryosurgery.
Observe Symptoms Your Patient Exhibits
A patient might present to the office without a hemorrhoid diagnosis, but symptoms such as rectal pain (K62.89, Other specified diseases of anus and rectum) or rectal bleeding (K62.5, Hemorrhage of rectum and anus) could give away the condition. During the office visit, the physician will usually perform an inspection of the external and she may add an anoscopy to look specifically for internal hemorrhoids or another cause of bleeding.
You would report the office visit with the following codes:
Sometimes the patient gets diagnosed with hemorrhoids in the course of undergoing another procedure. This is the case in our example where the patient comes for a screening colonoscopy during which the gastroenterologist notices internal hemorrhoids. Generally, unless they're causing a problem for the patient, the physician will leave the hemorrhoids alone, experts say. Usually a patient has to have a symptom, like rectal pain, for the GI doc to do anything about the hemorrhoids. The physician usually doesn't do anything with hemorrhoids unless the patient complains he is bothered by it.
You would report the example given above using the following codes:
Reminder: The Affordable Care Act statues provide that patients with average risk for colorectal cancer, aged 50 and above, whether Medicare or commercial payer, are entitled to a screening colonoscopy once every 10 years. For Medicare, you should bill non high-risk encounters with G0121 (Colorectal cancer screening; colonoscopy on individual not meeting criteria for high risk). For commercial payers the base procedure code would be 45378 (Colonoscopy, flexible; diagnostic, including collection of specimen[s] by brushing or washing, when performed [separate procedure]). For commercial payers, you would add modifier 33 (Preventive services), which was created to allow providers to identify to insurance payers and providers that the service was preventive under the applicable laws, and that patient cost-sharing does not apply.