Upgrade Your Fecal Microbiota Transplant Coding Skills
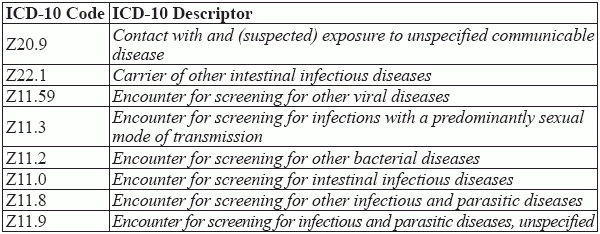
Billing Medicare? Understand the differences between 44705 and G0455. If your gastroenterology practice isn’t making use of fecal microbiota transplant coding (FMT), the odds are that it will within five years. While the FDA currently only allows FMT to treat Clostridium difficile infections (CDI) that don’t respond to standard treatments, it is very likely successful trials will make FMT widespread in coming years. Clinical trials are out there testing the microbiome’s impact on everything from weight loss to autism, so familiarizing yourself with the coding process is a proactive step for your practice. Quick clinical refresher: In FMT, the gastroenterologist transplants fecal bacteria from a healthy donor into a recipient to help the patient’s gut microorganisms repair or replace the disrupted native microbiota. The transplant can be done via colonoscopy, esophagogastroduodenoscopy or EGD, nasogastric or NG feeding tube, or rectal enema. Report Your Donor Collection Services If you are using a family member or local volunteer, then you’ll want to accurately reflect your work to collect the donor stool specimen, recommends Michael Weinstein, MD, president & CEO of Capital Digestive Care, Silver Spring, Md. To do that, you’ll report an appropriate level E/M code for the specimen collection so you’ll be reimbursed for that part of the process. While payers may vary on what ICD-10 codes they accept to reflect the donor encounter and the sample testing, the American Gastroenterological Association in its FMT coding guidance, suggests the following V and Z-codes, as appropriate: Distinguish Between Preparation and Instillation When your gastroenterologist performs a stool transplant, a significant step in the process is the sample preparation which includes assessing whether the donor specimen is suitable for transplanting. To report this service, you’ll use CPT® 44705 (Preparation of fecal microbiota for instillation, including assessment of donor specimen). Be aware of these three 44705 caveats: Look for Details on the Instillation Method In addition to the preparation of the donor specimen (reported using 44705), you will separately report the appropriate code for the instillation (placement) of the specimen in the gut, depending on which of the methods below the doctor uses: If physician places the specimen by oro-nasogastric tube or enema, use 44799 (Unlisted procedure, small intestine). Be aware that payers may not reimburse for this unlisted service. Openbiome.org Provides an Alternative for Fecal Transplant Material If donor samples are a challenge for you, there’s good news. Openbiome.org may provide a great workaround. “This non-profit organization works with clinicians to make FMTeasier, cheaper, safer and more widely available,” says Weinstein. “They provide hospitals and physicians with screened, frozen material ready for clinical use. This service eliminates the time, staff, protocols, and facilities needed to screen and prepare material from new donors for each treatment.” Resource: To find out more, go to http://www.openbiome.org/home/ When the notes indicate an esophagogastroduodenoscopy (EGD) placement, you’ll report 43235 (Esophagogastroduodenoscopy, flexible, transoral; diagnostic, including collection of specimen(s) by brushing or washing, when performed [separate procedure]). Example: If your gastroenterologist uses an EGD to instill the specimen, you should report 43235, along with 44705 for the preparation of the specimen. If your physician places the sample during a colonoscopy, report 45378 (Colonoscopy, flexible; diagnostic, including collection of specimen(s) by brushing or washing, when performed (separate procedure)). Payment factor: The 2017 fee schedule payment rate for 43235 is $129.56 for facility, $261.27 for non-facility; 45378 pays $195.23 for facility, $322.64 for non-facility. Billing Medicare? Heed This Instruction Code 44705 has a Medicare Physician Fee Schedule procedure status indicator of “I” (Not valid for Medicare purposes), so you should not report this code for FMT for Medicare beneficiaries; the costs for screening the donor specimen are typically not covered by Medicare. So, be prepared to provide an ABN to the donor and recipient beneficiary in this case. Instead, for Medicare benes, you’ll report HCPCS code G0455 (Preparation with instillation of fecal microbiota by any method, including assessment of donor specimen). G0455 includes both preparation and instillation work, so Medicare does not pay a separate fee for the installation of the microbiota by oro-nasogastric tube, enema, or by upper or lower endoscopy. Sample used? CMS will only reimburse for preparation and assessment of a fecal microbiota sample if the sample has been used in the treatment of the patient. Review 2 Summary Coding Scenarios: Example 1: To treat a 40-year-old patient with a C. difficile infection not responding to antibiotic treatment, your physician decides to use FMT. Using a specimen from the patient’s brother, he orders a thorough assessment of the stool sample to check for communicable diseases and other parasitic infections. He then prepares a sample for instilling in the patient’s gut. Your gastroenterologist then performs a colonoscopy to instill the stool sample. What to report: Example 2: A 70-year-old female patient with persistent CDI needs FMT; your physician performs the collection from her spouse, prepares the sample, and places it via EGD. Assuming this patient has Medicare coverage, for the sample collection and encounter, as well as the FMT preparation and instillation, you should report only G0455. ICD-10 for FMT: What’s Needed to Support Medical Necessity To reflect the reason the recipient had to have a fecal microbiota transplant, you’ll include the appropriate ICD-10 code (s) with 44705 or HCPCS code G0455 to support medical necessity. Currently, your choices are pretty limited where payer-approved diagnoses and FDA guidelines are concerned, confirms Weinstein. Many payers, including Aetna, are sticking with ICD-10 code A04.7, (Enterocolitis due to Clostridium difficile) as acceptable to report with 44705 and consider FMT “experimental” for such conditions as colon cancer, Crohn’s disease, diabetes, and functional gastro-intestinal disorders (e.g., irritable bowel syndrome, functional constipation, functional diarrhea, and functional dyspepsia). Watch this space: As FMT gains acceptance as a recognized treatment for conditions besides C. difficile, your payers may add other diagnoses and thus broaden coverage. “There are anecdotal reports of improvement for Ulcerative Colitis and Crohn’s Disease,” says Weinstein. “Clinical trials are ongoing in the U.S. and abroad. For now, though, stick with the only approved condition.”