Refresh Your Urgent Care E/M Understanding
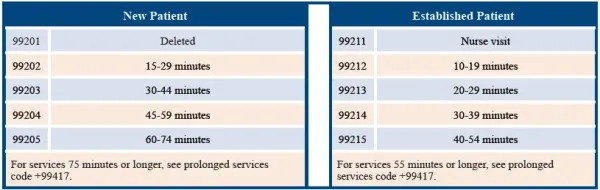
Here’s how UCC coding has, and has not, changed in 2021. If you’re familiar with emergency department (ED) coding, and your ED has expanded to include urgent care center (UCC) services as well, not only will you now have to make your way around the place of service (POS) codes, but you’ll also have to grasp the new office/ outpatient guidelines too. Here’s what you should be doing now that 2021 is in full swing. Refresher: UCCs are generally equipped to treat non-life-thr`eatening acute injuries and illnesses that do not require hospital admission. Most UCCs also provide other non-emergent services such as prescription refills, sports/school physicals, occupational health services, vaccinations, and STD testing. In addition, UCCs have recently become some of the most common sites for COVID-19 test administrations. Use Office E/M Codes for Services Outside the ED To code and bill E/M services in the urgent care setting, you will use office/outpatient E/M codes 99202-99205 (Office or other outpatient visit for the evaluation and management of a new patient …) and 99211-99215 (Office or other outpatient visit for the evaluation and management of an established patient …). CPT® defines a new patient as one “who has not received any professional services from the physician/qualified health care professional or another physician/qualified health care professional of the exact same specialty and subspecialty who belongs to the same group practice, within the past three years.” Therefore, if a patient sees Physician A (an ED provider) in the UCC setting in 2020 and returns in March 2021 to see Physician B (another ED provider), then that would be considered an established patient. Of note: This is different from how it would be in the ED setting, because the ED E/M code set (99281-99285) does not differentiate between new and established patients. Zero in on These Key E/M Component Differences Coders whose experience is mainly with ED E/M codes 99281-99285 should carefully review the CPT® guidelines for coding the outpatient E/M codes, as there are some differences — and the guidance for these codes just changed in January 2021. First: You can choose to report the appropriate code (99202- 99215) based on medical decision making (MDM) or on time alone, whether or not you meet the old requirement that counseling and/or coordination of care dominates the service. Second: The number of minutes included in the code descriptors changed for each code in the 99202-99215 range in 2021. Additionally, prior to January, time was used as a “typical” time. Instead, CPT® 2021 lists a total time range for each code. For instance, 99212 used to be a “typical” 10 minutes, but now the code identifies the total time range of 10-19 minutes. Third: You should select your code level based on time or the MDM — you don’t need both, says Rae Jimenez, CPC, CIC, CPB, CPMA, CPPM, CPC-I, CCS, senior vice president of product at AAPC and coding liaison to the AMA CPT® Editorial Panel. Total time could include face-to-face time, as well as time spent reviewing the chart before the encounter, time ordering diagnostics, coordinating care after the encounter, or even writing documentation — but not time spent by non-billable staff. A table with the time thresholds appears below: E/M code selection based on time: Scenario: A 42-year-old male established patient presents with a painful protrusion in the groin area. The urgent care physician examines the site, and has the patient stand and cough. Based on strangulation concern, the physician orders an abdominal ultrasound and discusses possible options based on the results. The doctor documents spending 45 minutes combined face-to-face time and research time related to the history and diagnostic testing but does not document the MDM thoroughly. Coding: Because CPT® 2021 allows you to select a code based on MDM or time, you can determine a level for this encounter based on time. The physician spent 45 minutes interacting with this established patient, counseling, and researching the situation, so you could report 99215 (Office or other outpatient visit for the evaluation and management of an established patient, which requires a medically appropriate history and/or examination and high level of medical decision making. When using time for code selection, 40-54 minutes of total time is spent on the date of the encounter) for the encounter. Remember: The medical record must reflect the provider’s actions during this 45-minute encounter. “At minimum, the total time spent on the day of encounter should be recorded, and an auditor should be able to review the note and see that the complexity of the problems dealt with would ‘logically’ entail that much time on the encounter date,” says Glenn D. Littenberg, MD, MACP, FASGE, AGAF, a physician and former CPT® Editorial Panel member in Pasadena, California. Don’t Forget the POS Code Is Different, Too Place of service for urgent care services can vary according to the payer guidelines and the specific characteristics of the UCC, so watch how you apply your POS indicator. You will use place of service (POS) codes 11 (Office), 20 (Urgent care facility), or 22 (On-campus outpatient hospital) as follows: 




.webp)
