Got Preventive Medicine Questions? We've Got Answers
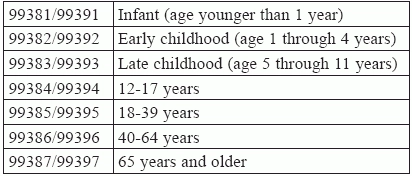
Know how to document and report separately with this handy FAQ. We all know that preventive care is a critical part of primary care. Yet, even though “preventive visits and vaccinations are just a few examples of ways people can stay healthy … Americans use preventive services at about half the recommended rate” according to the Centers for Disease Control and Prevention (CDC) (Source: www.cdc.gov/healthcommunication/toolstemplates/entertainmented/tips/PreventiveHealth.html). So, what better reason to refresh your understanding of the guidelines for reporting this valuable service. Simply study the definitive answers to these most frequently asked preventive E/M questions, and you’ll be a preventive medicine coding expert in no time. Question: What is a preventive medicine visit, and how is it documented? Answer: Though the CPT® guidelines note that “the extent and focus of the services will largely depend on the age of the patient,” preventive medicine visits such as 99381-99387 (Initial comprehensive preventive medicine evaluation and management of an individual …) or 99391-99397 (Periodic comprehensive preventive medicine reevaluation and management of an individual …) are comprised of the same basic elements, tailored to the age and gender of the patient: As the guidelines preceding these codes in CPT® note, the “comprehensive” nature of codes 99381-99397 reflects an age- and gender-appropriate history/exam and is not synonymous with the “comprehensive” examination required in E/M codes 99201-99350. Also, some interventions, such as immunizations, are separately reportable. Your provider’s notes will need to document all of the above. Additionally, CPT® guidelines require that “pre-existing problems and trivial problems or abnormalities encountered during the preventive medicine visit that do not require additional work should be noted but not reported,” as Mary I. Falbo, MBA, CPC, CEO of Millennium Healthcare Consulting Inc. in Lansdale, Pennsylvania, points out. Coding alert: The preventive medicine E/M codes are all age-specific, so make sure you assign the correct code for your patient. Question: What kinds of screening, testing, and vaccinations are usually performed during a preventive visit? Answer: Naturally, “that will depend on the age and gender of the patient,” Kent Moore, senior strategist for physician payment at the American Academy of Family Physicians, explains. “What a provider screens, tests, and vaccinates for on a 6-month old female will be radically different from that for a 60-year old male,” Moore goes on. “For example, an infant female could require testing for developmental delays and an IPV, inactivated poliovirus, vaccination, while the older male could require a prostate cancer screening and a vaccination for shingles,” Moore elaborates. A good place to find out what kinds of screenings, counseling, and vaccinations should be a part of a preventive medicine visit for older patients is this guide prepared by Medicare: https://www.medicare.gov/Pubs/pdf/10110.pdf Question: What happens if a preventive medicine E/M reveals a problem? Answer: CPT® guidelines are very specific about this: an “insignificant or trivial problem/abnormality that is encountered in the process of performing the preventive medicine evaluation and management service and which does not require additional work and the performance of the key components of a problem-oriented E/M service should not be reported,” as Falbo noted previously. However, should the visit uncover a significant problem, CPT® directs you to report a problem oriented E/M service from 99201-99215, appending modifier 25 (Significant, separately identifiable evaluation and management service by the same physician or other qualified health care professional on the same day of the procedure or other service) to show that the service was distinct from the preventive medicine visit. Question: What else can be reported separately from 99381/99397? Answer: Any vaccines administered during the exam (as well as their administration) can be billed in addition to the preventive medicine codes providing they have a valid CPT® or HCPCS. So, for example, you can separately report and bill CPT® codes for immunization administration and vaccine risk/benefit counseling such as 90460 and +90461, codes for immunization administration without counseling (90471-+90474), vaccine/toxoid products such as90476-90749, hearing tests, and fecal occult blood tests. However, CPT® guidelines do not allow you to separately report counseling and risk-factor reduction interventions such as 99401-99404 (Preventive medicine counseling and/or risk factor reduction intervention(s) provided to an individual …) or 99411-99412 (… in a group setting …), Moore explains. Question: Are preventive visits covered by insurance? Answer: This is very much up to the individual payers. If they do cover preventive visits, they will often only allow one per year, and they may not cover all the services that such visits should entail. So, it is very important that you know exactly what your patient’s health plan allows.