Big changes will impact this diagnosis, for dates of service April 1 and beyond.
As the coronavirus emergency has brought new patients to the ED, it’s also delivered unexpected coding challenges amid rapidly changing regulations and updated coding guidance every week. One area where EDs are getting conflicting information involves diagnosis coding.
To ensure that you’re applying the right codes and sequencing them properly, consider the following expert tips from Betty Ann Price, BSN, RN, president and founder of Professional Reimbursement and Coding Strategies, and an AHIMA-approved ICD-10-CM trainer.
DOS Key to Choosing Right Diagnosis Codes
One of the biggest hurdles for EDs who are looking for the right diagnosis coding advice is understanding how the rules change based on the date of service (DOS), Price says.
Here’s why: Although EDs had been using B97.29 (Other coronavirus as the cause of diseases classified elsewhere) when seeing COVID-19 patients, the ICD-10-CM Coordination and Maintenance Committee decided on an emergency insertion of a new, more specific code to address COVID-19 during its meeting on March 17-18: U07.1 (COVID-19).
“The speed that the ICD-10-CM Coordination and Maintenance Committee approved this new code is unprecedented,” Price says. “The new code, U07.1, was initially assigned by the World Health Organization. Usually it requires at least a one-year process to get a new code adopted, but this went through with exceptional speed. In addition, the code was initially scheduled to go into effect on October 1, but during the meeting, they decided to make it effective as of April 1, 2020, instead,” she notes.
With the new code now made official, consider these tips on how to code once you know the dates of service.
For Claims With Dates of Service Through March 31, 2020:
If you’re coding a chart for a coronavirus patient with a date of service on or before March 31, 2020, you’ll code the manifestation of the illness first, followed by code B97.29 for the COVID-19, Price says. B97.29 must be listed after the manifestation(s) of the disease. The manifestation will be the primary code for these dates of service, she says.
For example, Price advises, if a patient came in on March 20 with viral pneumonia and tested positive for COVID-19, you would first report J12.89 (Other viral pneumonia), followed by B97.29.
If the patient instead has bronchitis due to COVID-19, use code J40 (Bronchitis, not specified as acute or chronic) first, followed by B97.29, (Other coronavirus as the cause of diseases classified elsewhere) as the secondary code.
For Dates of Service on Or After April 1, 2020:
When seeing patients with dates of service on or after April 1, you will use U07.1 as your primary or principal diagnosis code, with the manifestation coded afterward, Price says. “This sequencing change is the biggest difference between the two dates of service, and something you must be aware of,” she notes. “U07.1 needs to be the primary code even above respiratory distress or respiratory failure — you must put that U code first with dates of service April 1 or after.”
Therefore, taking the viral pneumonia patient example from above, you would report U07.1 as your primary code, followed by J12.89. “So it’s the same viral pneumonia code, but this time viral pneumonia is the secondary code,” Price says.
One rationale for reporting the U code first is that, as with all the temporary federal waivers in place for coronavirus reimbursement, it will be important for payers to see the coronavirus code at the front of your claim, which will unlock many of these special payment circumstances, she says.
Don’t Forget Z Code Options
If a patient presents to the ED suspecting that they might have coronavirus, but it’s ruled out by either exam/evaluation and/or by testing, you should use a Z code instead of the coronavirus codes, Price says. These codes should be used for all dates of service — they are not affected by the new U07.1 code addition. These codes are:
“You’ll use Z20.828 when there is confirmed exposure to another COVID-confirmed person — someone else who tested positive to have coronavirus,” Price says. “But the patient you’re seeing is asymptomatic. This is used as part of the epidemiological survey in trying to track the contacts.”
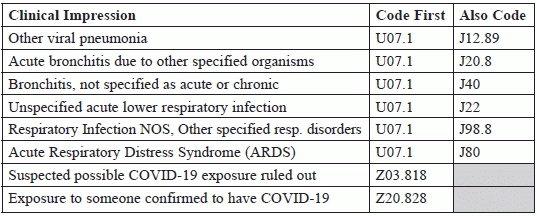
Price put together a chart (see above) for the American College of Emergency Physicians to show how to report coronavirus with other manifestations after April 1, 2020.
Source: The American College of Emergency Physicians: https://www.acep.org/globalassets/images/covid-19-coding-update-march-18-2020.pdf.
Scour the Medical Record
ED coders should review the medical record carefully, particularly for patients who have respiratory symptoms, Price says. “Coders will be looking to see if patients have been tested, or whether coronavirus is considered,” Price says. “Everyone who walks into an ED right now is suspect, so it will involve careful review to determine whether or not the COVID-19 is ruled out by evaluation and/or testing, and whether or not the COVID-19 test was positive.”
Use This New Code for Coronavirus Tests
If you test a patient for coronavirus, you can use the new CPT® Category I Pathology and Laboratory code 87635 (Infectious agent detection by nucleic acid (DNA or RNA); severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (Coronavirus disease (COVID-19)), amplified probe technique). This code went into effect on March 13, 2020. Keep in mind that this is an early release code, so you may need to manually upload this code descriptor into your electronic health record system.
