Your coding will likely depend on your physician roster.
A patient reporting to the ED with symptoms of stroke will test the ED’s ability to evaluate the patient quickly and decide the best course of treatment. Claims for these patients will test the coder’s ability to identify all the elements (and codes) that could be involved when your physician treats a patient with stroke symptoms.
In order to code optimally, coders will need to be able to identify different evaluation and management (E/M) and imaging coding options. Further, expertise on selecting stroke diagnosis codes will come into play.
Read on to recognize the codes you’ll need to report stroke cases.

Symptoms of Stroke Include Vision Changes
A cerebrovascular accident (CVA), also known as a stroke or cerebral infarction, occurs when the patient experiences a disruption in the blood flow to the brain. When the blood flow is interrupted, the brain cells don’t receive the nutrients and oxygen needed from blood and begin to die within a short amount of time.
Common signs that a patient has experienced a stroke include:
Note Locale on E/M
A stroke patient, like all undiagnosed patients, will undergo an E/M service so the physician can assess the patient prior to any further testing.
Due to the severity of the condition, the ED physician will likely see their share of patients with stroke symptoms. When this occurs, you’ll likely code the E/M with a code from the 99281 (Emergency department visit for the evaluation and management of a patient that may not require the presence of a physician or other qualified health care professional) through 99285 (Emergency department visit for the evaluation and management of a patient, which requires a medically appropriate history and/ or examination and high level of medical decision making) code set or 99291 (Critical care, evaluation and management of the critically ill or critically injured patient; first 30-74 minutes) and +99292 (… each additional 30 minutes (List separately in addition to code for primary service)).
Dx Determined Via Imaging
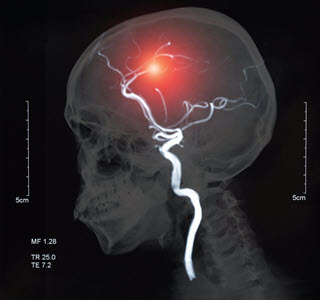
When the patient presents to the ED to receive care for a possible stroke, healthcare professionals have several imaging modalities at their disposal to detect and diagnose the condition.
The imaging options available for diagnosing a CVA include, but are not limited to:
Each imaging modality has its own benefits. For example, NCCT scans are ideal for imaging immediately after the provider has stabilized the patient. NCCT is used to help exclude hemorrhagic stroke and can identify calcification, which makes it possible to detect lesions.
A provider may perform a duplex US to screen for carotid artery stenosis if the patient is suspected to have experienced a stroke.
Modifier alert: Since all of the ED physician’s imaging services will be performed using facility equipment, be sure to append modifier 26 (Professional component) to any imaging test performed.
Make Sure Your Physician Ordered and Interpreted Imaging
Verify that the imaging studies listed above were actually ordered and interpreted by your emergency physician rather than someone else before coding the interpretation with modifier 26 (Professional component) appended. Remember that in the 2023 CPT® medical decision making (MDM) table that Category 1 data points have changed to allow ordering and interpreting each diagnostic test. You may also claim Category 2 data points for independent interpretations of a test, rather than relying on the radiologist’s interpretation of that imaging.
Category 3 points can be earned if the emergency physician has a discussion with the radiologist or neurologist regarding the management or test interpretation
Take Stroke Dx to Furthest Character
If you receive a report that states the provider diagnosed the patient with a stroke or CVA, the ICD-10 code set has several code options available in the I63.- (Cerebral infarction) code category. The following code subcategories allow you to assign an appropriate code for a CVA diagnosis where the physician identifies the cause of the stroke:
Except for I63.6, each code subcategory listed above can be further expanded to a 5th and sometimes 6th character to complete the codes. You’ll use a 6th character in the I63.0- to I63.5- code subcategories to specify the circulatory structure affected and laterality.
If the provider documents a stroke or CVA without any additional information, you’ll assign the default code of I63.9 (Cerebral infarction, unspecified). This code features an additional synonym of “Stroke NOS,” which stands for not otherwise specified and lines up with the provider’s diagnosis.
Pay Attention to the Parent Code Notes
The I63.- code category features two notes instructing you to use additional codes if certain criteria are met. One note directs you to use Z92.82 (Status post administration of tPA (rtPA) in a different facility within the last 24 hours prior to admission to current facility) to identify that the patient was administered tissue plasminogen activator (tPA) or recombinant tissue plasminogen activator (rtPA) at a different facility before being admitted to the current facility.
“tPA is used quickly after stroke onset to help restore blood flow to brain regions by dissolving blood clots blocking blood flow. rtPA has been considered the standard of care for treatment of acute ischemic stroke,” says Kristen Taylor, CPC, CHC, CHIAP, associate partner of Pinnacle Enterprise Risk Consulting Services in Centennial, Colorado. According to Z92.82’s descriptor, the tPA or rtPA administration must have occurred within the previous 24 hours in a different facility for you to accurately report the code.
The other “use additional code” note instructs you to assign the appropriate National Institutes of Health Stroke Scale (NIHSS) score from the R29.7- (National Institutes of Health Stroke Scale (NIHSS) score) subcategory.
