Quick charts teach how to “G” code for multiple possibilities.
If you’re behind the curve on CMS’ latest blood pressure quality measure, you could sideline your PQRS pay. Here’s the lowdown on screening your patient population for high blood pressure – and how you can zap through the G codes to know which choice is best.
(See Chiropractic Coding & Compliance Alert, Vol. 1, No. 2 for instructions on reporting pain assessment and functional assessment measures.)
Learn About the Measure
CMS added quality measure 317 (Preventive care and screening: Screening for high blood pressure and follow up documented) in 2014. The measure is intended to encourage providers to collect data when screening patients for high blood pressure. It also tracks whether the provider completes the requisite follow-up documentation on patients with blood pressure higher than normal. “It’s to show the quality and continuity of care across the disciplines” says Doreen Boivin, CPC, CCA, with Chiro Practice, Inc., in Saco, Maine.
During each visit the provider has to report:
a. Whether he screened a patient for high blood pressure.
b. Whether he documented an appropriate care plan for patients with blood pressure higher than normal.
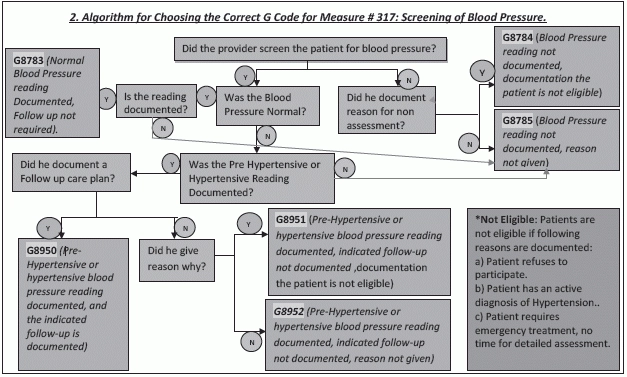
c. The appropriate G code (See Fig. 2 for deciding on the right “G” code for you.)
Providers who report Measure 317 should screen patients for hypertension at least once per reporting period and subsequently work out a follow-up as required. Patients with hypotension or low blood pressure are not recommended for a follow-up.
The blood pressure readings can be classified in to four categories: normal, pre-hypertensive, first hypertensive, or second hypertensive (See Fig. 1).
What happens next: Based on the reading, the provider may prescribe at least one lifestyle modification such as weight reduction, the Dietary Approaches to Stop Hypertension (DASH) eating plan, dietary sodium restriction, increased physical activity, or moderation in alcohol consumption. These modifications are recommended by the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC).
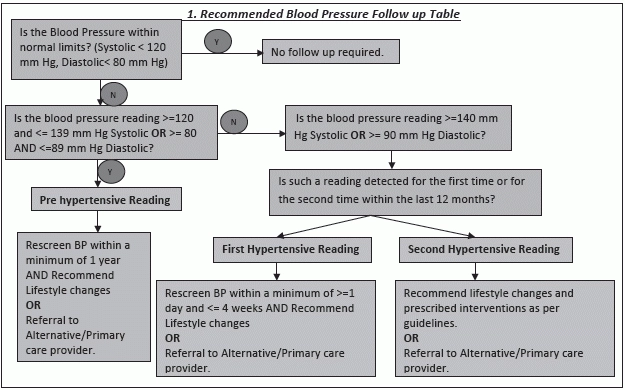
The “second hypertensive” reading refers to the patient getting a hypertensive reading for the second time, after having first tested hypertensive within the last twelve months. In such a case, interventions according to JNC must include at least one of the interventions that include hypertensive pharmacological therapy, laboratory tests, or an electrocardiogram (ECG).
Brush Up On G Code Basics
CMS established G codes as part of HCPCS to report data when calculating quality measures. These codes supplement the claim documentation by measuring the quality of services provided. You could choose to report the G code that best describes the services provided and whether documentation was appropriate.
Future implications: The measures that CMS is tracking currently could be the forerunners of future criteria to prove necessity of care and determine whether providers receive adequate reimbursement. Also, participating in quality measure reporting shows a dedication to the delivery of quality care, thus reassuring patients that their providers are committed to their best interests.
Here are two flow charts to help you through with decision making in this measure. The first chart tells you the course of action you need to take as per the patient findings and the second chart goes all the way to fix a G code for all the case scenarios possible.
