Reader Questions:
Modifiers That Help Bill Noncovered Services With ABN
Published on Fri Jun 12, 2015

Question: Are the providers required to bill “noncovered” services to Medicare when requested by the beneficiary? What modifiers apply, if any?
Texas Subscriber.
Answer: Yes, providers do need to bill the services as per the request of the beneficiary. Here are the various modifiers you may need to use:
-
Modifier GY is used when “noncovered” services such as X-rays, massage, ultrasound, and physical therapy are performed by a chiropractor and the provider elects to bill those services to Medicare. Claims billed with this modifier will be automatically denied by the Medicare claims processing system and the beneficiary will be liable for all charges, whether personally or through other insurance.
-
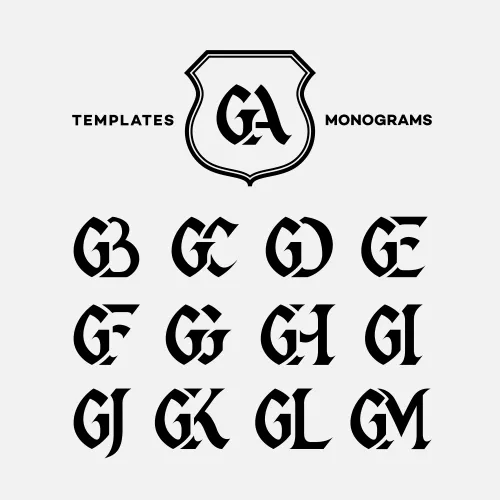
Modifier GA is used when the provider has issued a valid ABN (advance beneficiary notice) for maintenance care and the beneficiary has selected Option 1. This modifier may also be used on assigned claims when a patient refuses to sign the ABN and the latter is properly witnessed. When using the modifier GA, it must be appended to the spinal manipulation CPT® code. If no modifier is appended to the spinal manipulation codes, the claim will deny in the system as not medically necessary.
-
Modifier GZ is used in those rare cases when the provider expects that Medicare will deny an item or service as not reasonable and medically necessary but the provider did not obtain a valid ABN prior to the services being rendered.
-
Modifier AT (acute treatment) must be appended to the chiropractic manipulation code to indicate the manipulation was for medically necessary and reasonable treatment of an acute subluxation or chronic subluxation as defined in national policy and LCD L27350. The AT modifier should not be placed on the claim when maintenance therapy has been provided. Claims without the AT modifier will be considered as maintenance therapy and denied.