Cardiology Coding Alert
Discover What's New For Cardiology in the CCI Policy Manual

Don't miss the new secondary percutaneous transluminal thrombectomy instruction.
You've learned all about the new 24.0 Correct Coding Initiative (CCI) updates in past issues of Cardiology Coding Alert. But, how much do you really know about the 2018 CCI Policy Manual For Medicare Services?
Along with the CCI edits, it's important to read the manual, according to Ruby Woodward, BSN, CPC, CPMA, CPB, COSC, CSFAC, CPC-I, coding and compliance manager at Suburban Imaging/Suburban Radiologic Consultants in Minneapolis, Minnesota.
Updates to the manual happen annually, and those changes are noted in red, Woodward adds.
Section D of chapter 5 contains more than 45 items you must remember when submitting your cardiology claims. Read on to learn more about the additions this year.
Don't Overlook New Thrombectomy Instruction
Specific to cardiology services, the manual has added clarity and a case example for secondary percutaneous transluminal thrombectomy reporting in the updated 2018 manual in chapter five on page V-18, under item 28, according to Cynthia A. Swanson, RN, CPC, CEMC, CHC, CPMA, senior manager of healthcare consulting for Seim Johnson in Omaha, Nebraska.
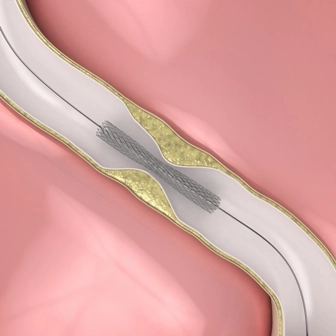
The impacted code in this item is: +37186 (Secondary percutaneous transluminal thrombectomy (eg, nonprimary mechanical, snare basket, suction technique), noncoronary, non-intracranial, arterial or arterial bypass graft, including fluoroscopic guidance and intraprocedural pharmacological thrombolytic injections, provided in conjunction with another percutaneous intervention other than primary mechanical thrombectomy (List separately in addition to code for primary procedure)).
The manual gave clarification that as of January 1, 2018, thrombectomy of a thrombus in a vascular territory of a diseased artery is inherent in the work of the atherectomy procedure, explains Theresa Dix, CCS-P, CPMA, CCC, ICDCT-CM, coder/auditor of East Tennessee Heart Consultants in Knoxville, Tennessee.
"CPT® code +37186 can no longer be reported for removal of a thrombus of a vessel treated with atherectomy," Dix adds.
The manual offers this case example for clarification: "For example, if a physician performs a lower extremity endovascular revascularization atherectomy, removal of any thrombus from the vascular territory of the vessel treated with atherectomy is not separately reportable."
Atherectomy defined: "When an atherectomy is provided, a catheter designed for lesion cutting is advanced across the blockage site," says Christina Neighbors, MA, CPC, CCC, Coding Quality Auditor for Conifer Health Solutions, Coding Quality & Education Department, and member of AAPC's Certified Cardiology Coder steering committee. "This catheter cuts away pieces of the blockage and stores these pieces in a section of the catheter prior to removing from the body. Sometimes not all of the pieces are retrieved, therefore, a follow-up thrombectomy is provided to successfully complete the intended/ordered procedure."
Note: A cutting balloon is not an atherectomy procedure supply and must be coded as an angioplasty procedure, Neighbors adds.
"Code +37186 refers to arterial thrombectomy when not initially planned," according to Neighbors. "This would be reported when an angioplasty or stent placement is performed and completion angiography shows an occlusion (thrombus) within another vessel requiring catheter thrombectomy, snare, or suction pump (manual or mechanical) removal. This code may also be reported when thrombectomy is performed prior to the intended ordered interventional procedure."
Caution: The physician's documentation must be accurate and support the additional secondary thrombectomy interventional procedure, Neighbors adds.
Notice Brand-New Addition to Items 38 and 39
Although the manual did not add another entirely new item to the cardiology section, it did make updates to a few existing items.
"With the annual AMA CPT® code changes, effective January 1, 2018, the NCCI Policy Manual for Medicare Services routinely incorporates applicable AMA revisions," Swanson says. "For example, in Chapter V, Surgery: Respiratory, Cardiovascular, Hemic and Lymphatic Systems (CPT® codes 30000-39999), page V-21, outlines a update in items 38 and 39, to reflect the 2018 AMA coding changes made to the reporting of chest X-ray services."
The additional codes the manual added in the examples to items 38 and 39 are as follows:
- 71045 (Radiologic examination, chest; single view)
- 71046 (Radiologic examination, chest; 2 views).
"When a central venous catheter is inserted, a chest X-ray is typically performed to confirm the position of the catheter and absence of pneumothorax," Swanson says. "The chest X-ray -- new 2018 CPT® codes 71045 (Radiologic examination, chest; single view), 71046 (Radiologic examination, chest; 2 views), 71047 (Radiologic examination, chest; 3 views), and 71048 (Radiologic examination, chest; 4 or more views) -- is part and partial to the CPT® code for the central venous catheter insertion."
Similarly, when the cardiologist performs a procedure like 93503 (Insertion and placement of flow directed catheter (eg, Swan-Ganz) for monitoring purposes), he often performs a chest X-ray after the 93503 service to confirm proper placement and positioning of the flow-directed catheter, Swanson adds. So, you would not additionally report a chest X-ray code like 71045 or 71046 with the Swan Ganz placement.
Reminder: Pre and/or post standard diagnostic procedure like electrocardiograms(EKGs) and X-rays that are provided without new symptoms/indications and are only provided to verify a physician's work or possible questionable complicationareincluded within the primary procedure, according to Neighbors.
"If a standard protocol diagnostic procedure is provided without signs and symptoms and something is found, that doesn't mean it's appropriate to charge," Neighbors adds. "The follow-up diagnostic procedure would be appropriate to capture as long as an order and ordering diagnosis support it."
Examples when not to report: The patient's pre-procedure and/or post-procedure EKG on a planned or scheduled cardioversion or ablation procedure. Post-procedure X-rays to verify lead placement or pneumothorax after lung biopsy are included within the primary procedure because these are standard protocol services provided to patients.
Example when to report: The physician performed a lung biopsy, and the initial standard procedure follow-up X-ray identified pneumothorax. Two hours later, a follow-up X-ray is provided on the pneumothorax found on the initial standard follow-up X-ray. The two hours later X-ray would be appropriate to report as long as an order and ordering diagnosis supports it, according to Neighbors.
Resource: You can find the CCI Policy Manual for Medicare Services at https://www.cms.gov/Medicare/Coding/NationalCorrectCodInitEd/index.html as the last file under "Downloads."
Related Articles
Cardiology Coding Alert
- ICD-10:
Pinpoint Your Atherosclerosis Codes With This Advice
Hint: Make sure you know if the patient also has angina pectoris. If you see [...] - 2018 Update:
Discover What's New For Cardiology in the CCI Policy Manual
Don't miss the new secondary percutaneous transluminal thrombectomy instruction. You've learned all about the new [...] - ICD-10:
Select Correct ICD-10 Codes for These Cardiology Diagnoses
Hint: Report I47.1 for paroxysmal supraventricular tachycardia. To ethically maximize your cardiology practice's bottom line, [...] - You Be the Coder:
Watch the Calendar With G0250
Question: Can you please explain the time limit for G0250? We have experienced some recent [...] - Reader Question:
Turn to 93924 for Noninvasive Physiologic Studies
Question: The cardiologist assesses the patient's blood flow in the arteries of his legs before [...] - Reader Question:
93619 or 93620? Know the Difference
Question: If the cardiologist tries to induce arrhythmia but fails, should we report 93619 or [...]