KELLEYB
New
Is anyone having an issue with Humana paying 71271 with ICD-10 Z87.891? We are billing professional only with a 26 modifier. We have been paid up until December and now claims are denying for DX code.
Is anyone having an issue with Humana paying 71271 with ICD-10 Z87.891? We are billing professional only with a 26 modifier. We have been paid up until December and now claims are denying for DX code.
This is for Medicare products.Is this for commercial or Medicare? I only ask because I was looking up the Medicare coverage info to see if there were any recent changes, and it occurred to me that you might be talking about a commercial plan instead.
(We don't really have any commercial Humana in my area - it's pretty much all Medicare, so my instinct for Humana is always to jump right to looking up Medicare policies/LCD/NCD.)
It should never have been ordered and should neve have been performed. The provider failed to order according to guidelines, and the imaging facility failed to screen according to guidelines. Someone's eating the cost of the LDCT. Maybe the patient turned 78 after the physician ordered the LDCT. Unlikely, but possible. Even then, not certain Medicare would cover it.There is an age restriction with Medicare: According to CMS, "71271 to be billed only if the beneficiary is between the ages of 50 and 77 for claims with date of service on or after February 10, 2022."
If the beneficiary is older than 77, how is this supposed to be billed out?
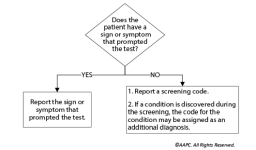
I submitted a code edit question to them and Humana is referencing this policy which states the Z87.891 cannot be in the primary position on the claim.
Medicare will deny G0296 and 71271 for claims that do not contain these ICD-10 diagnosis codes:
- Z87.891 for former smokers (personal history of nicotine dependence).
- F17.21 - for current smokers (nicotine dependence).
- F17.211 Nicotine dependence, cigarettes, in remission
- F17.213 Nicotine dependence, cigarettes, with withdrawal
- F17.218 Nicotine dependence, cigarettes, with other nicotine-induced disorders
- F17.219 Nicotine dependence, cigarettes, with unspecified nicotine-induced disorders